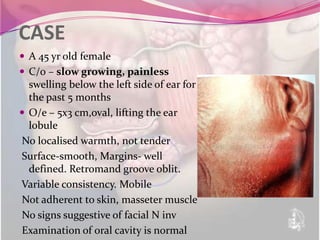
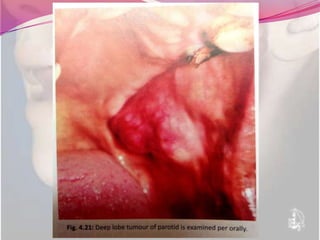
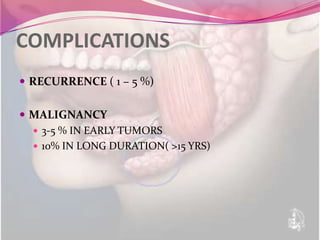
Pleomorphic adenoma is the most common benign tumor of the parotid gland. It consists of both epithelial cells and spindle-shaped mesenchymal cells within an abundant mucoid matrix. On pathology, it displays well-differentiated epithelial cells and spindle/stellate cells in a pleomorphic stroma with mucoid material. The tumor presents as a slow-growing, painless swelling of the parotid gland and is diagnosed by FNAC. The treatment is complete surgical excision via superficial parotidectomy while preserving the facial nerve. Recurrence is possible if there are pseudopods left behind or inadequate margins. Malignant transformation may occur in long-standing tumors.