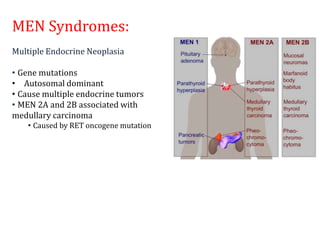
Thyroid nodules are abnormal growths in the thyroid gland that affect approximately 50% of the population. While most nodules are benign, thyroid cancer can develop in around 5% of cases. The main types of thyroid cancer are papillary, follicular, medullary, and anaplastic. Papillary carcinoma is the most common type, making up around 80% of thyroid cancers. It often spreads via lymphatic vessels and has an excellent prognosis with treatment. Follicular carcinoma also has a good prognosis but is more likely to metastasize hematogenously. Medullary carcinoma develops from parafollicular cells and can be hereditary. Anaplastic carcinoma is the most aggressive and