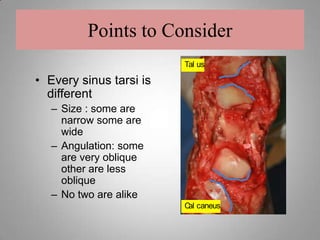
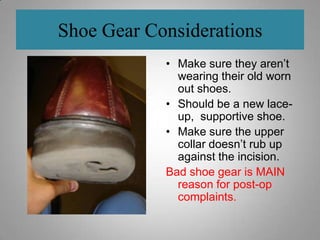
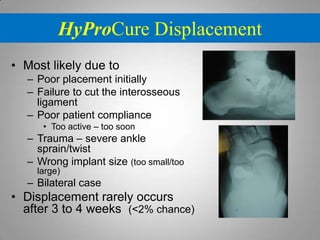
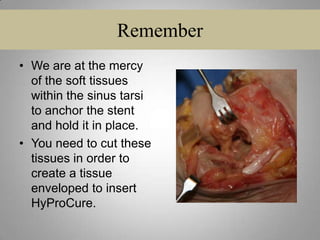
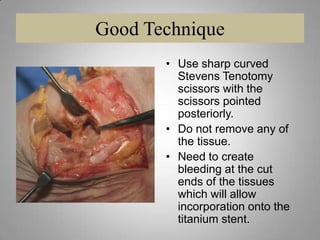
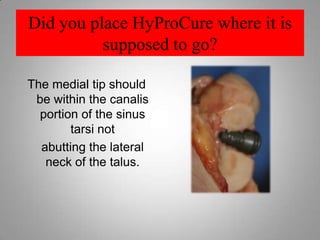
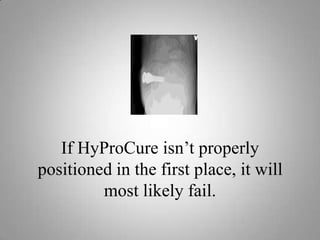
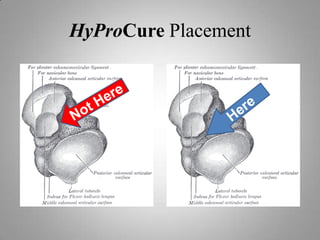
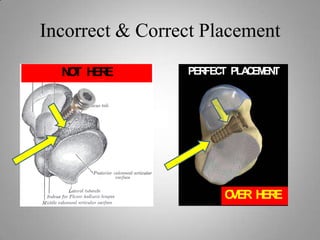
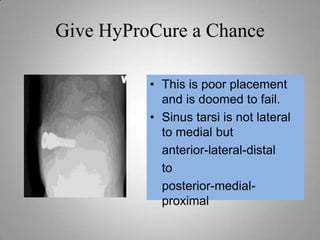
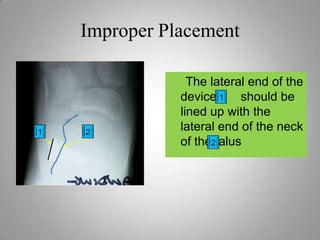
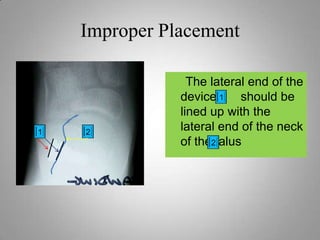
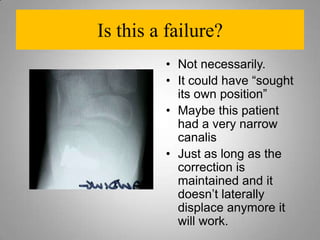
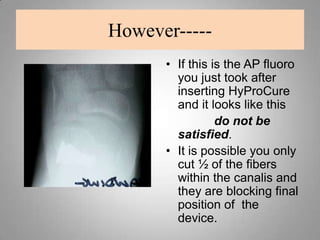
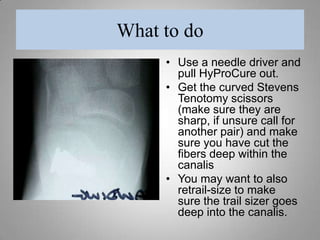
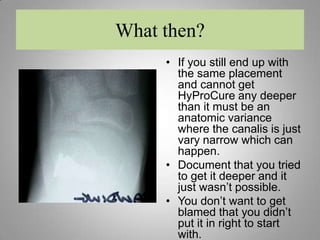
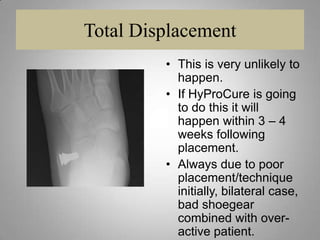
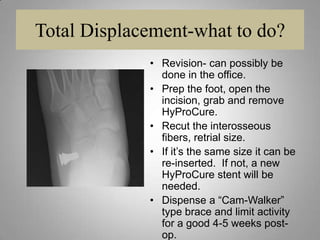
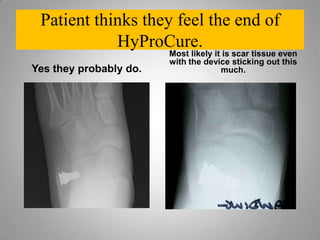
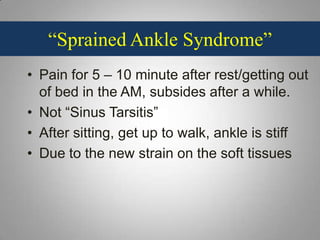
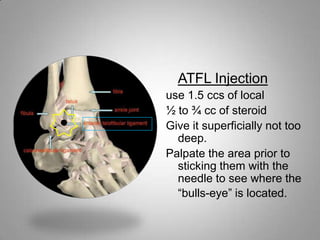
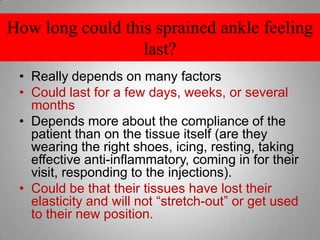
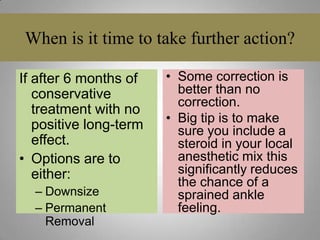
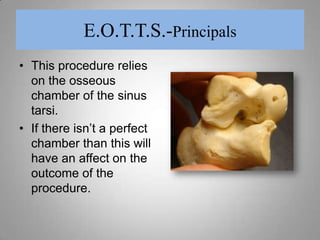
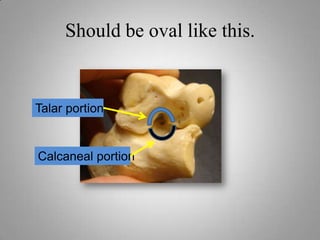
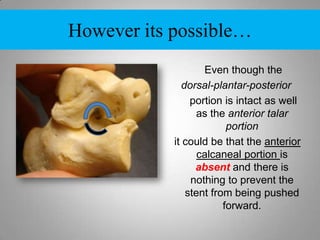
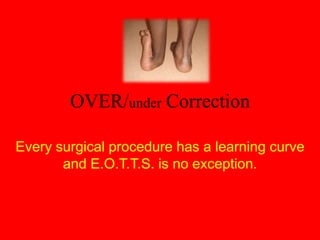
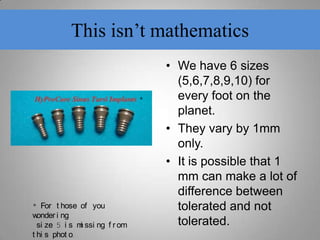
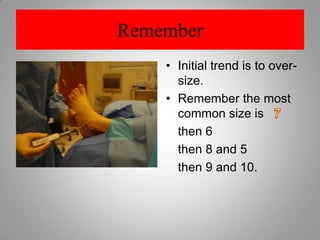
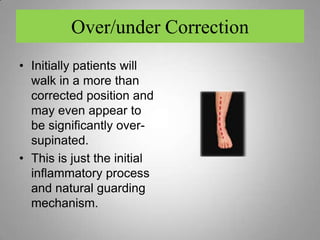
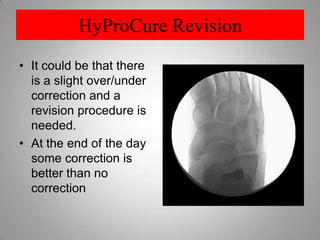
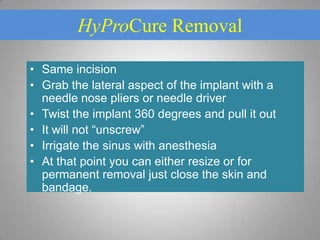
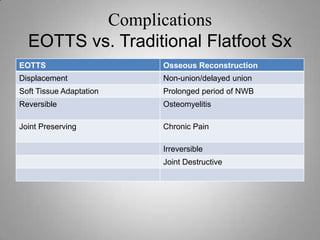
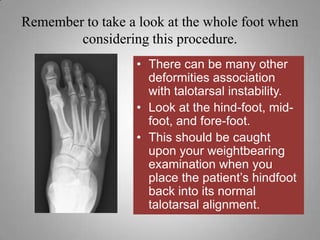
The document discusses the challenges and considerations associated with extra-osseous talotarsal stabilization surgery, highlighting the importance of proper placement of the hyprocure device, patient-specific factors, and postoperative care. It outlines potential complications arising from poor technique or patient non-compliance, as well as strategies for managing issues such as stent displacement and 'sprained ankle syndrome.' The text emphasizes that while complications can occur, the overall risk for severe outcomes is lower with hyprocure compared to traditional surgical methods.