1) Liver trauma is the second most common organ injured in blunt abdominal trauma and the most common injured in penetrating trauma, occurring in 1-8% of patients with multiple blunt trauma.
2) The liver is susceptible to injury due to its size, friable parenchyma, thin capsule, and fixed position near the ribs and spine.
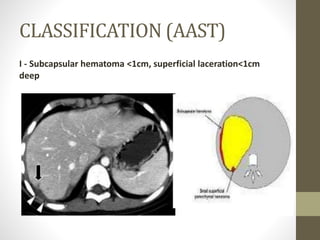
3) Liver injuries are classified based on the mechanism of injury, type and degree of damage, localization within liver lobes/segments, and whether associated vessels or bile ducts are damaged. Grades I-II are minor injuries while Grades III-V require surgical intervention and Grade VI is incompatible with survival.