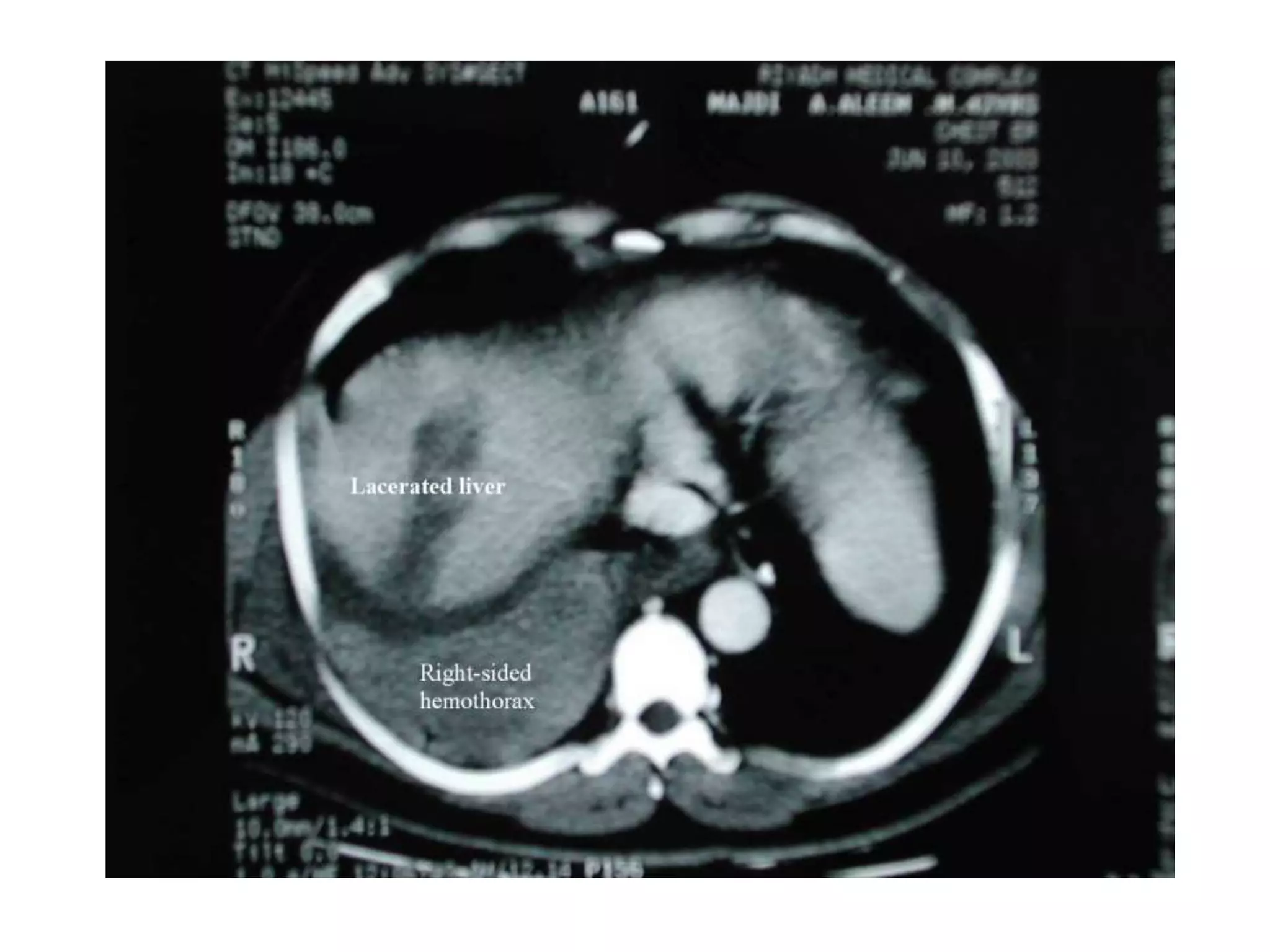
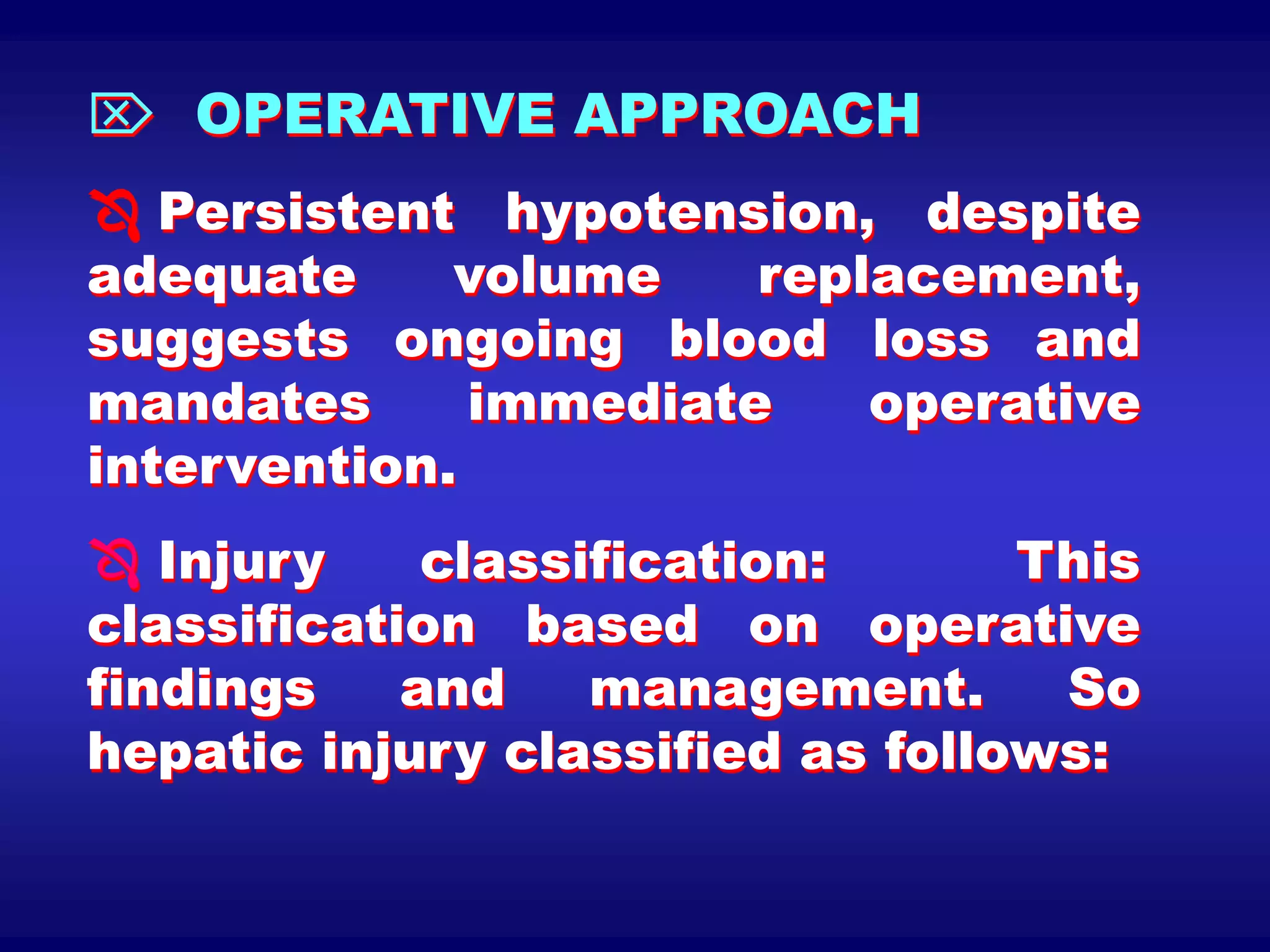
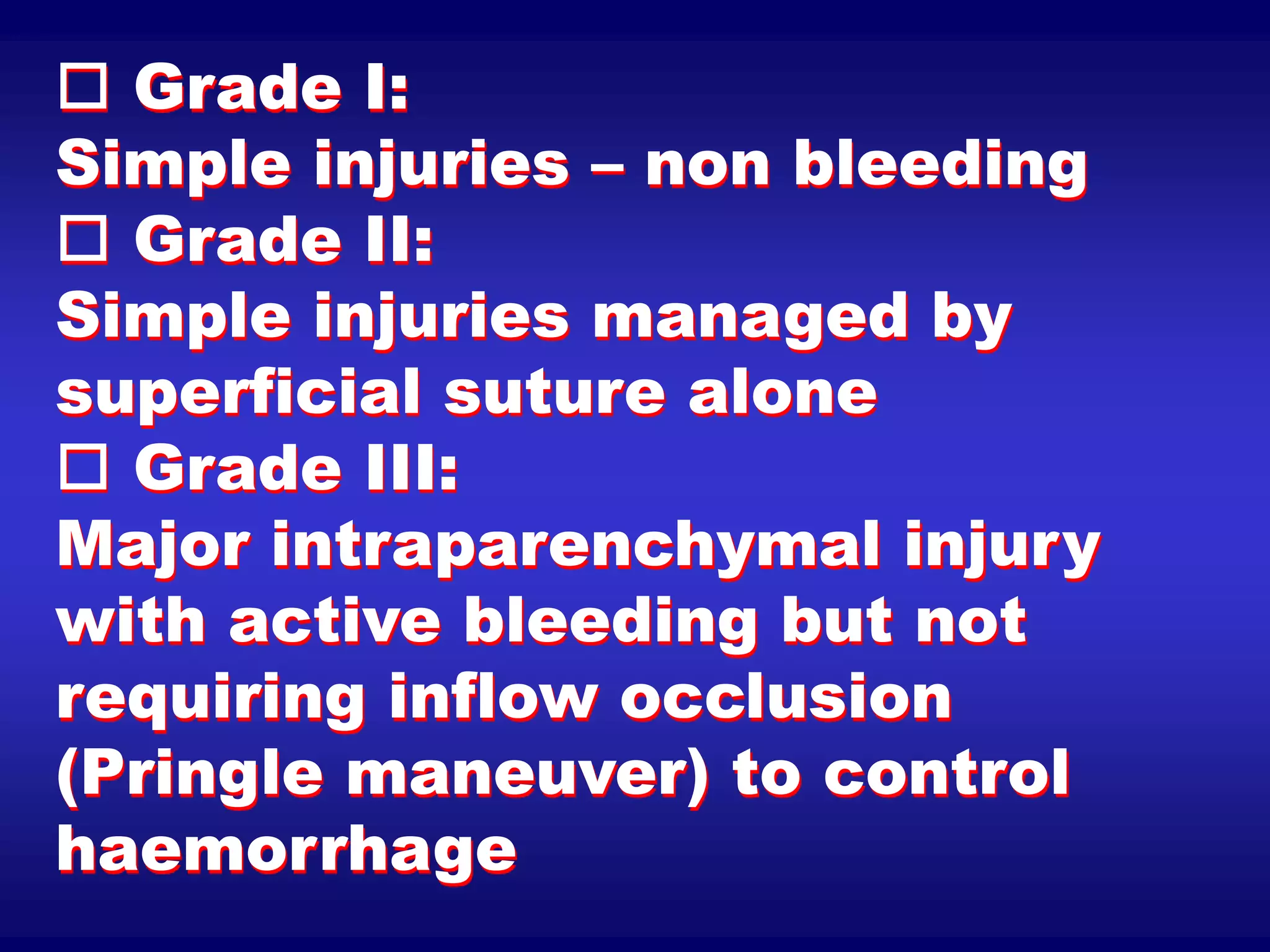
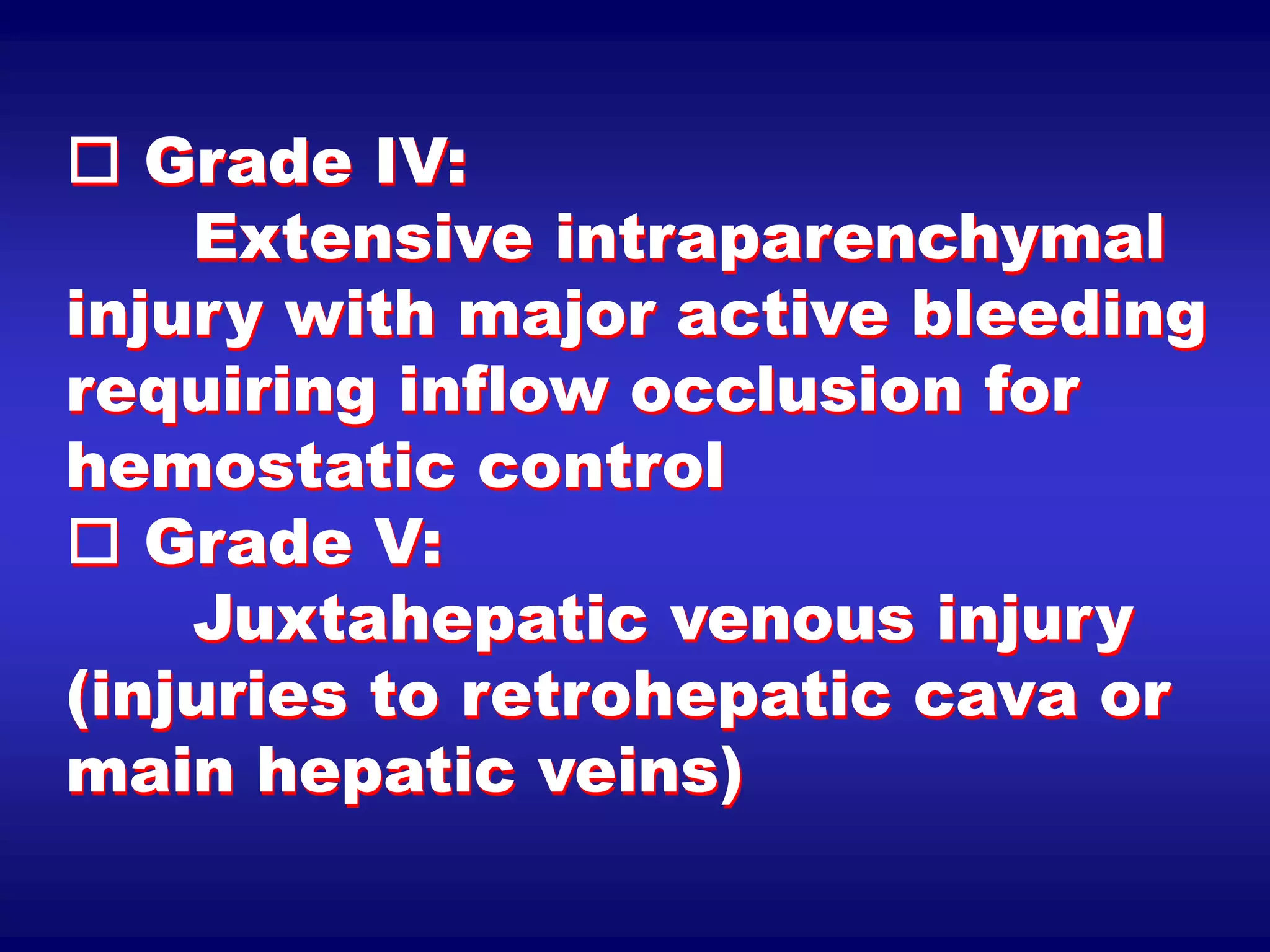
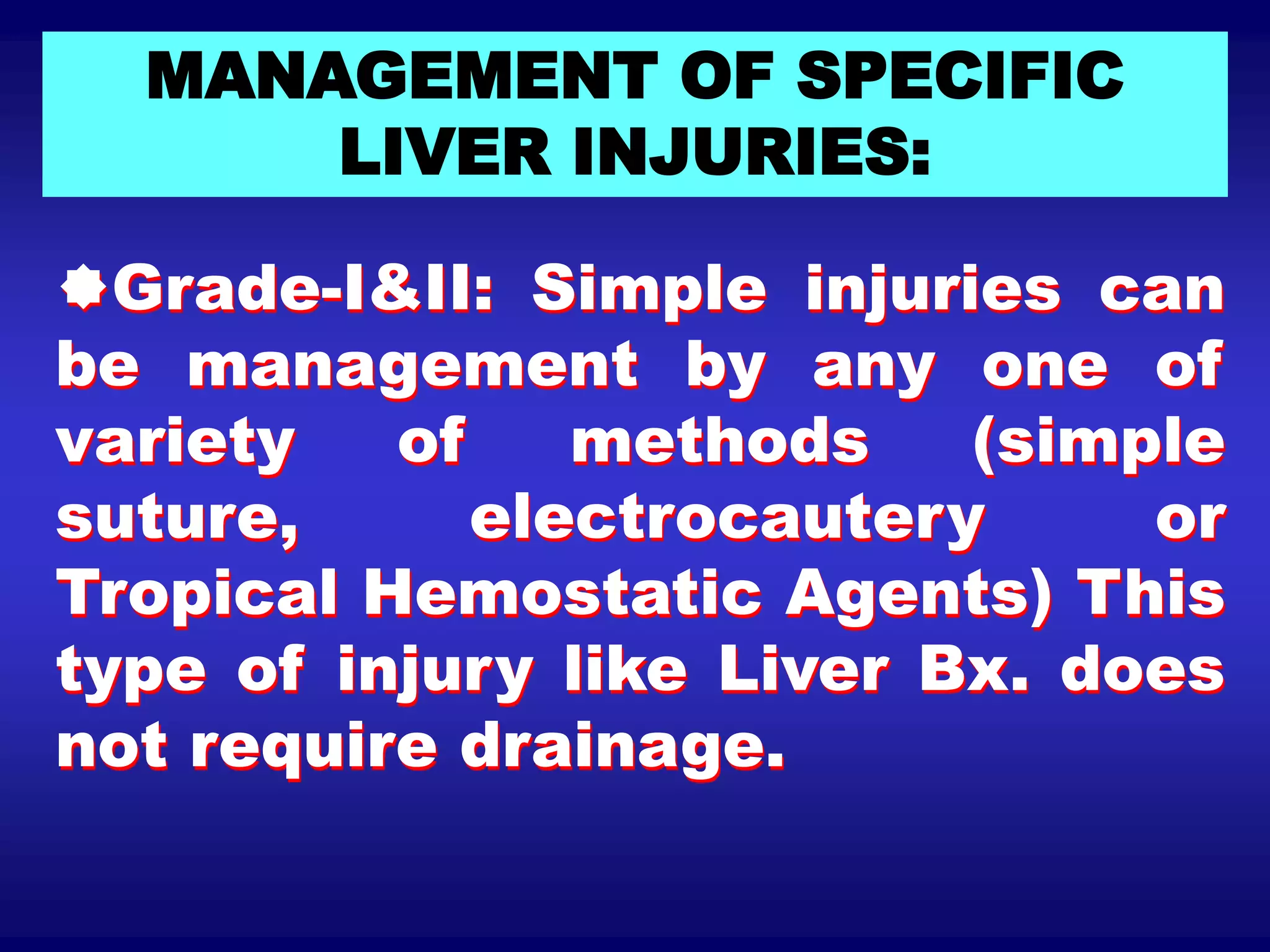
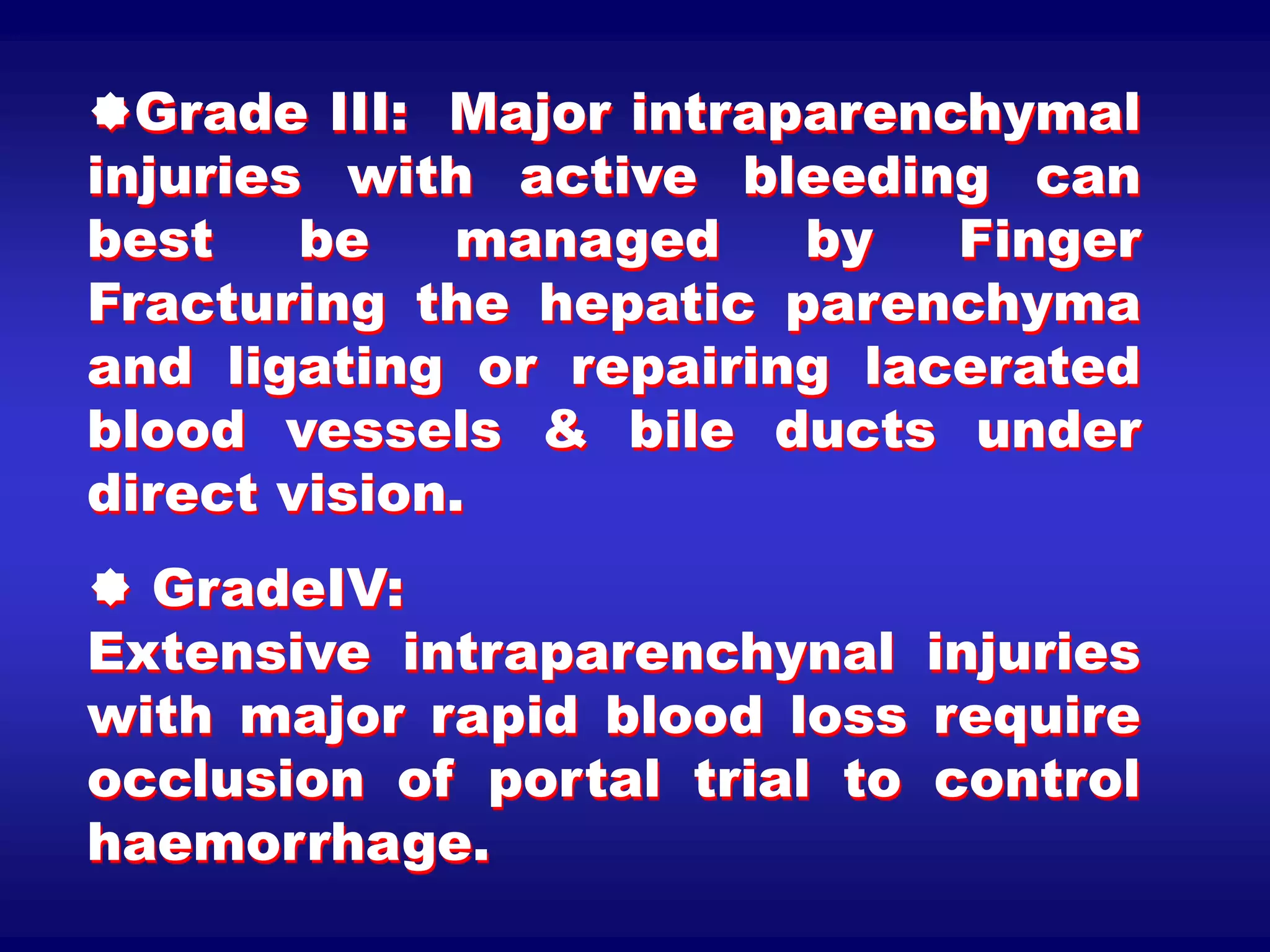
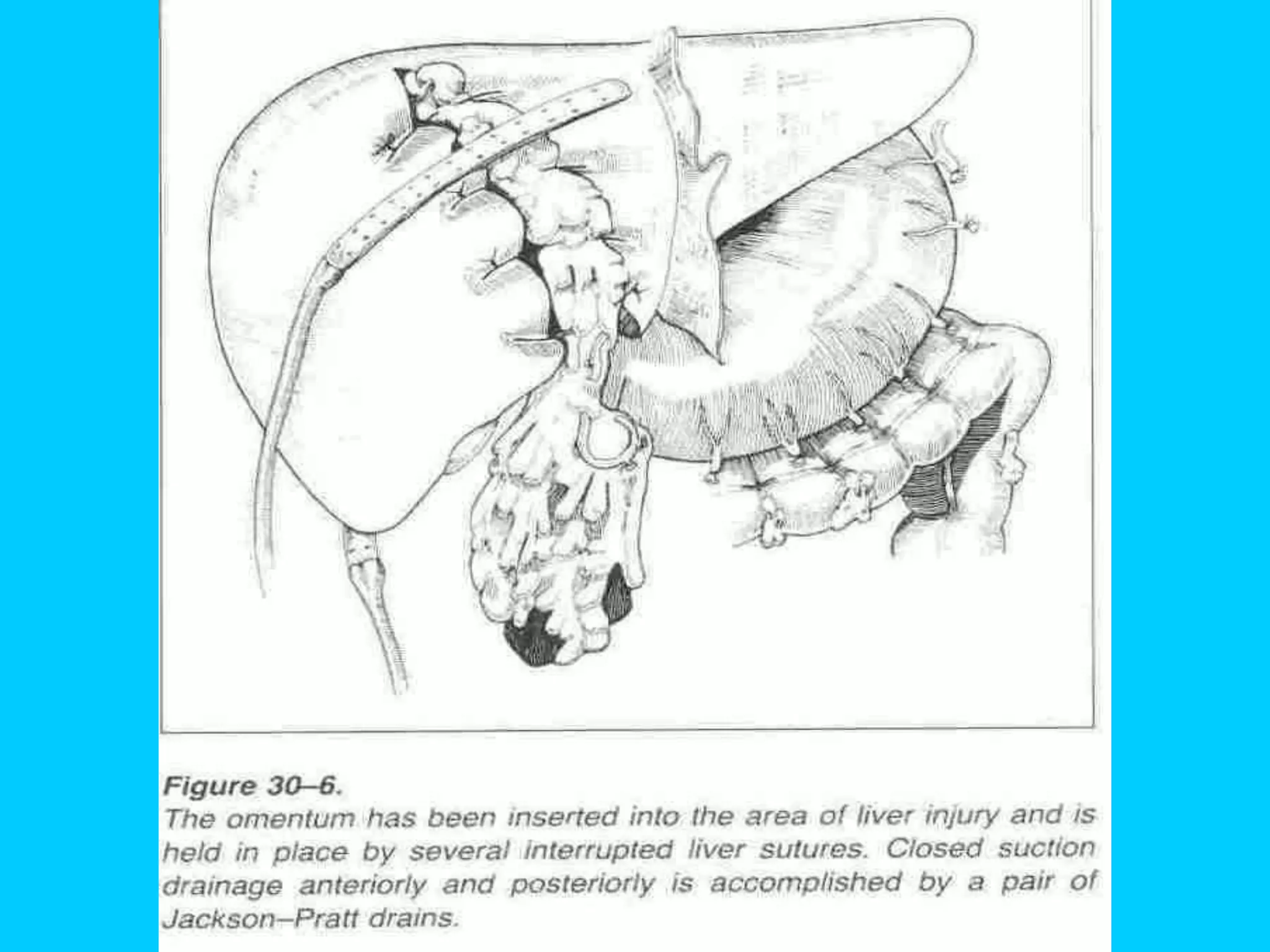
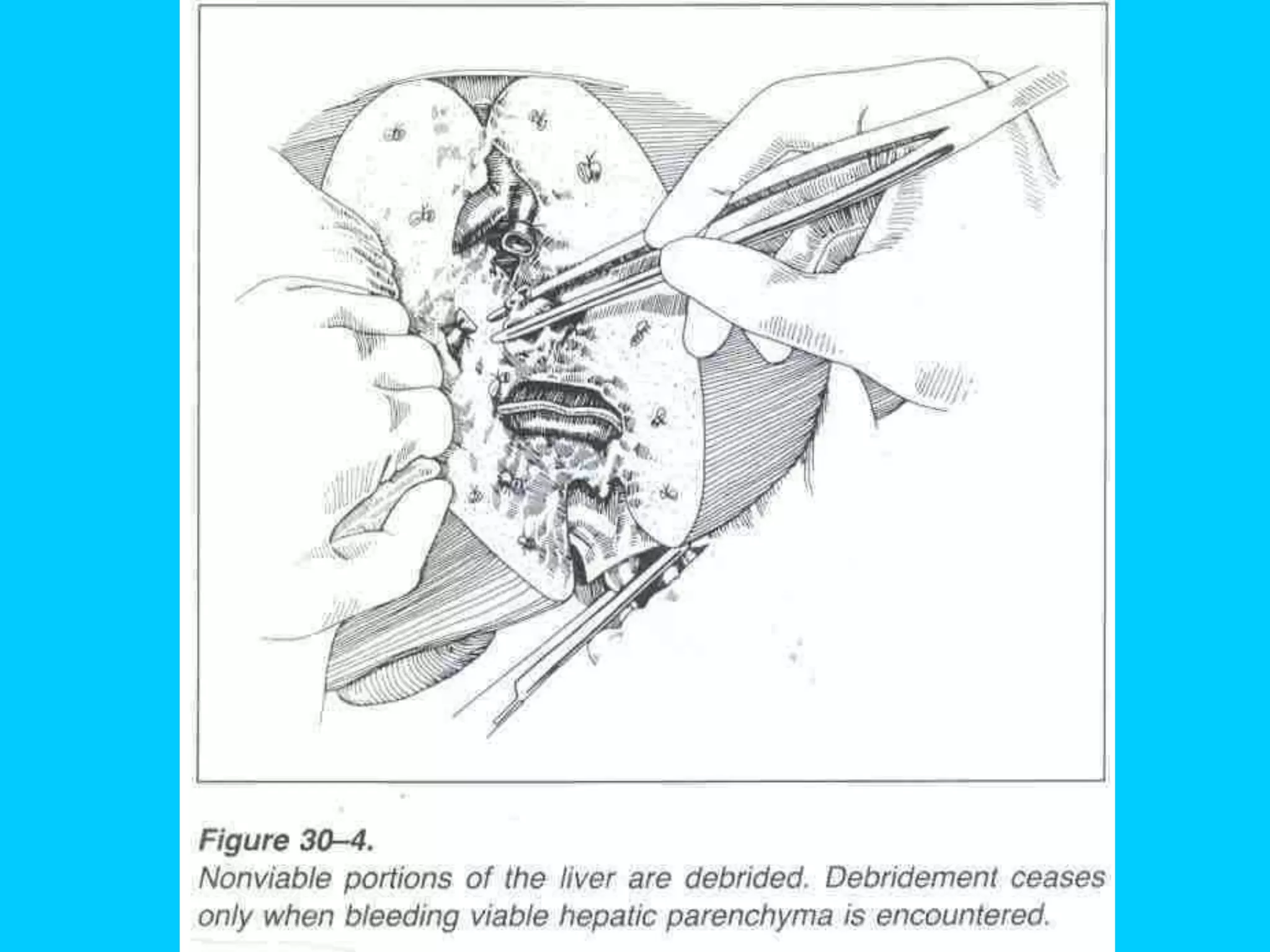
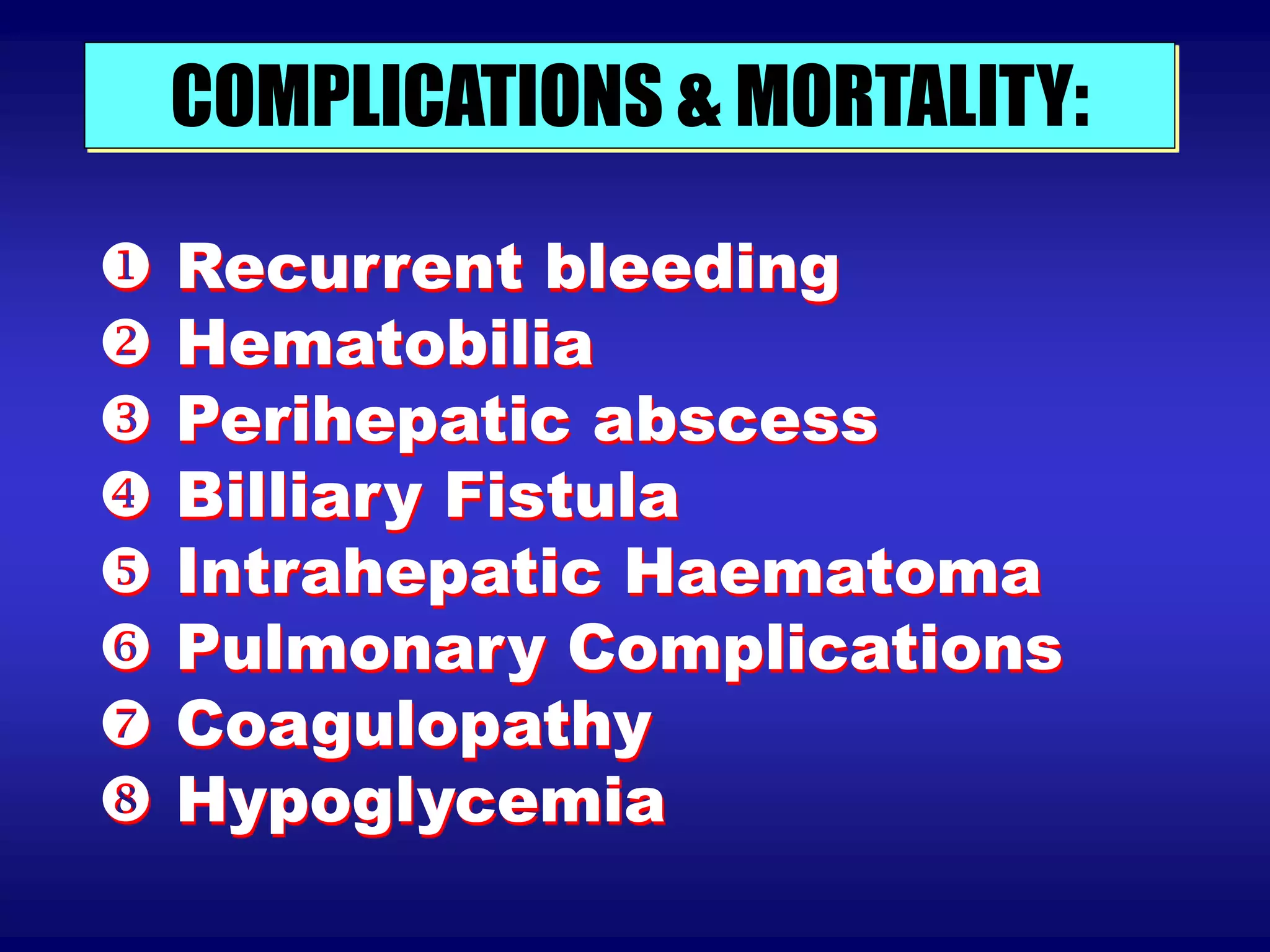
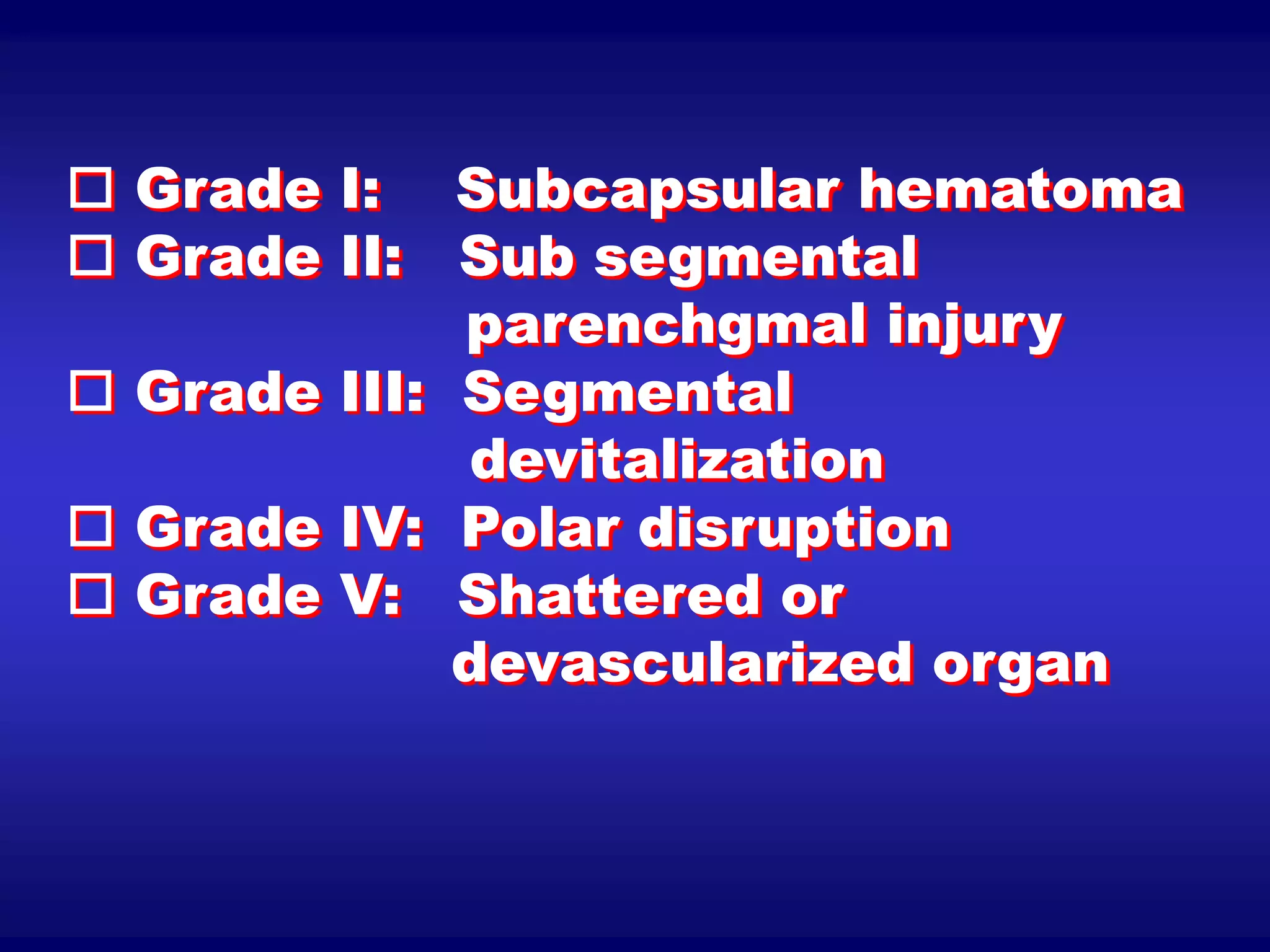
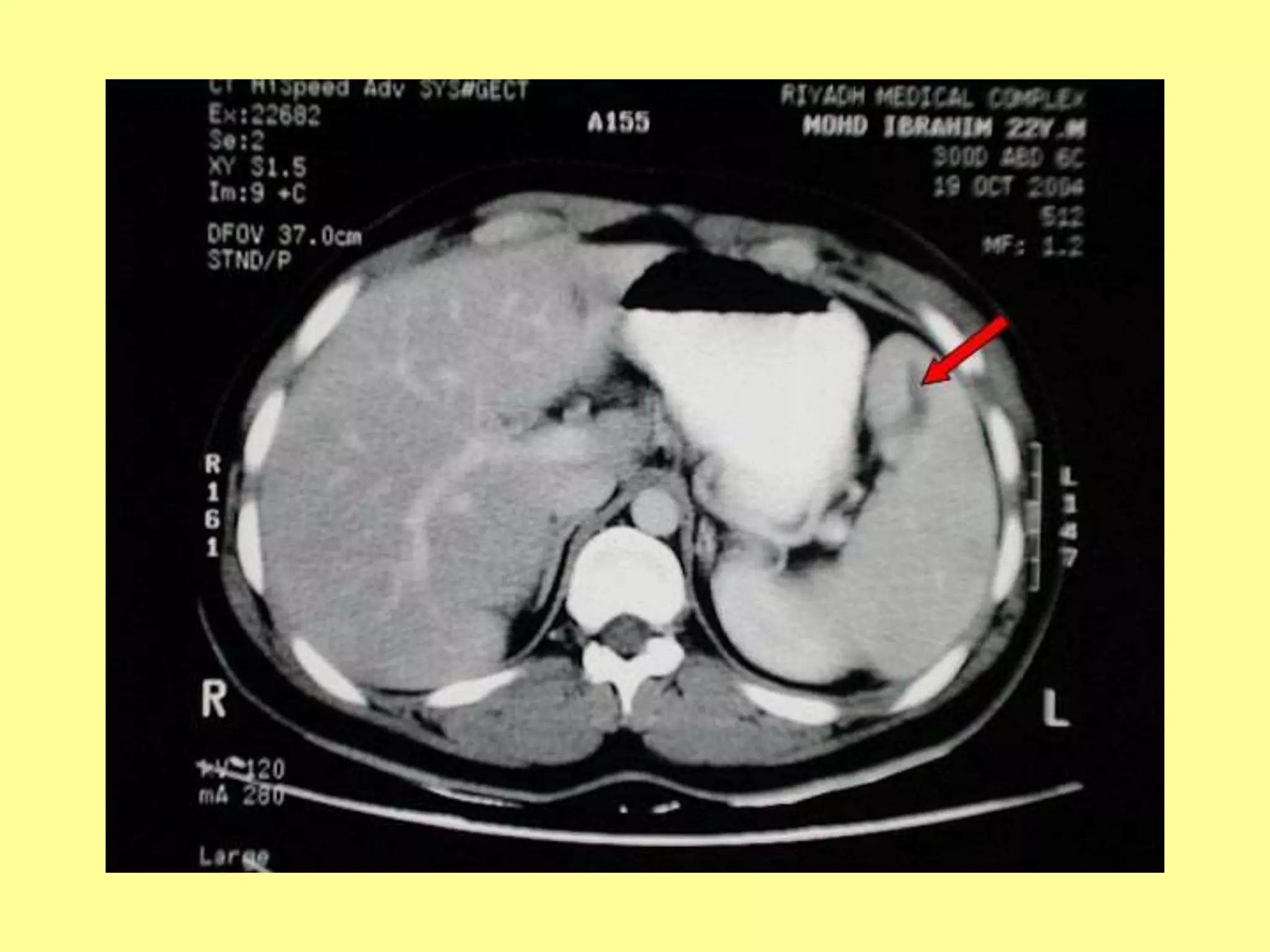
The document discusses abdominal trauma, focusing on injuries to the liver and spleen. It describes how the liver is most commonly injured in blunt trauma while the spleen is frequently injured in both blunt and penetrating wounds. For diagnosis, history, physical exam, diagnostic peritoneal lavage, CT scan, and laparoscopy may be used. Treatment depends on injury severity but may include observation, suturing, packing, or resection. Complications can include recurrent bleeding, infection, and organ-specific issues like hematobilia.