This document summarizes information about liver trauma, including:
- Epidemiology of liver injuries, which often occur with other injuries like spleen or rib fractures.
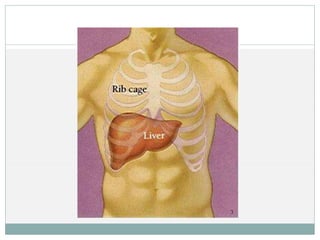
- Relevant anatomy of the liver, including its large size, friable tissue, and location making it prone to blunt trauma.
- Classification system for grades of liver injuries from 1 to 6 based on severity.
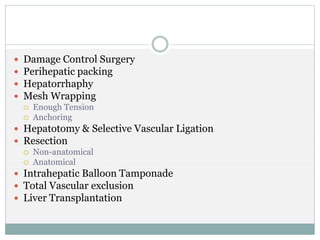
- Modern management primarily involves conservative non-operative treatment using CT scans and angiography, reserving surgery for more severe bleeding or injuries.
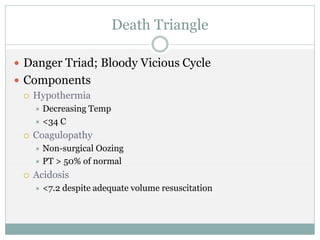
- Key concepts discussed are damage control surgery, the "death triangle" of hypothermia, coagulopathy and acidosis to avoid, and total vascular exclusion for severe bleeding control