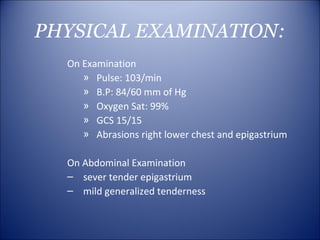
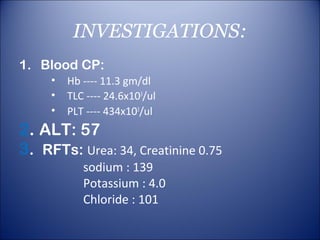
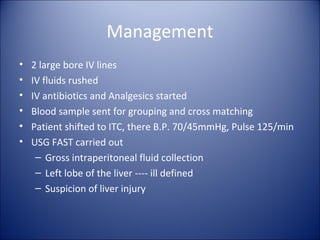
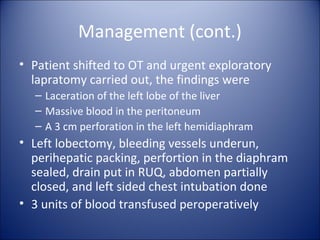
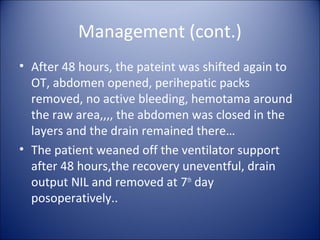
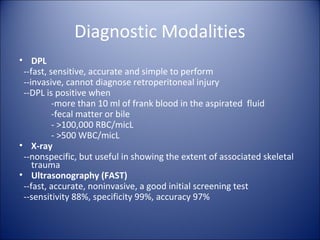
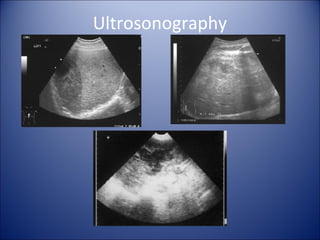
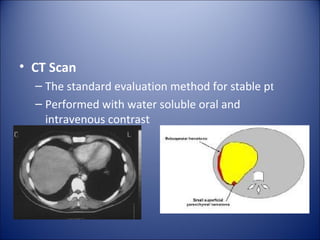
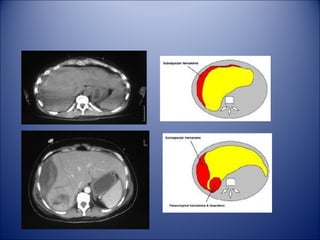
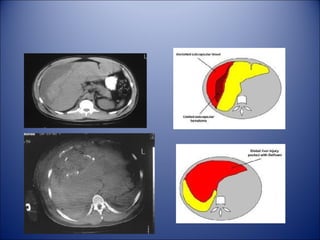
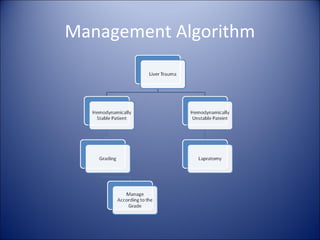
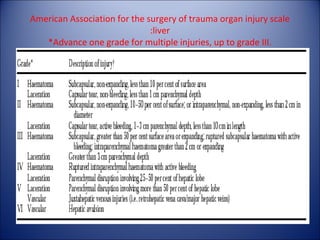
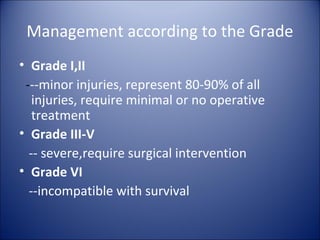
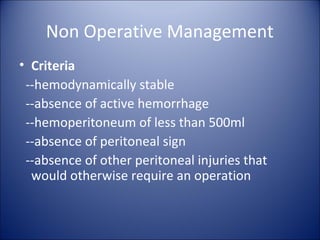
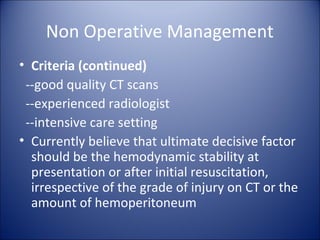
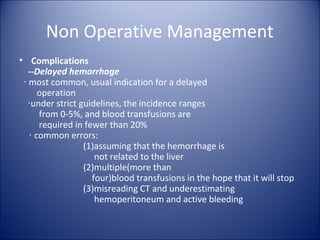
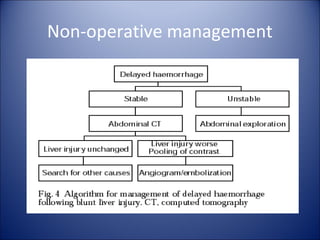
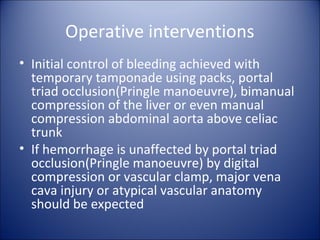
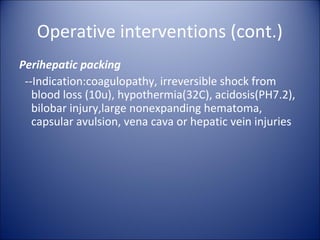
This document presents a case of traumatic liver injury in a 17-year old male patient who was in a motorcycle accident. He presented with abdominal pain and vomiting. Imaging showed a liver laceration and bleeding in the abdomen. He underwent an exploratory laparotomy where a left lobe liver laceration and diaphragm perforation were found and repaired. He recovered well after surgery with drain removal after one week and was discharged. Traumatic liver injuries can range from minor injuries treated non-operatively to severe injuries requiring surgery like lobectomy or packing to control bleeding. Both non-operative and surgical management were discussed.