1. Enterocutaneous fistulas are abnormal connections between the gastrointestinal tract and skin that allow intestinal contents to drain onto the skin. They most commonly originate from the small intestine.
2. Management of enterocutaneous fistulas involves stabilization of the patient, controlling sepsis, providing adequate nutrition, defining the anatomy of the fistula, and creating a treatment plan.
3. Key steps in management include fluid resuscitation, controlling fistula output, protecting the skin, draining any abscesses, providing nutrition either enterally or parenterally, and using pharmacological agents like octreotide to help reduce output.









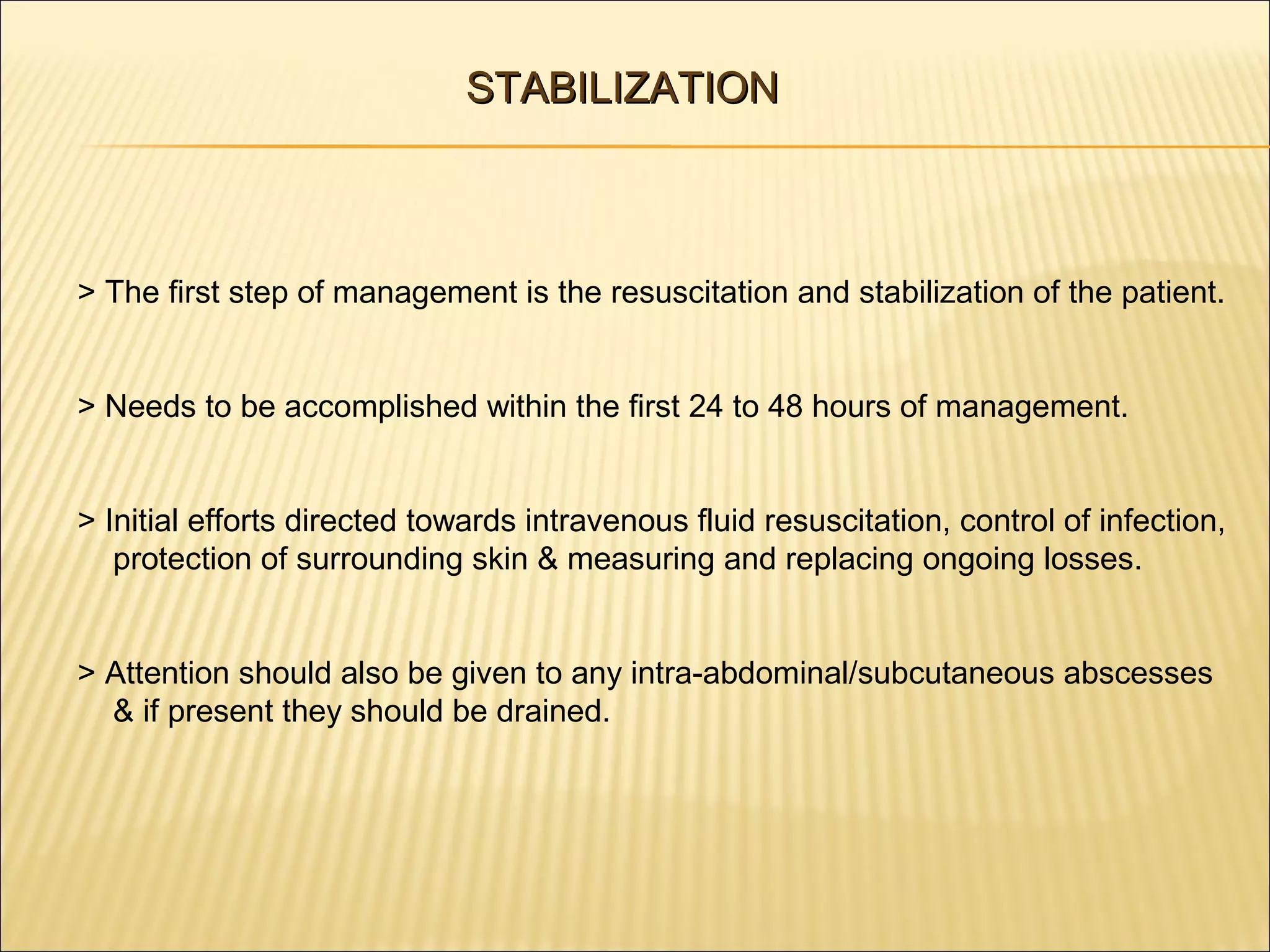





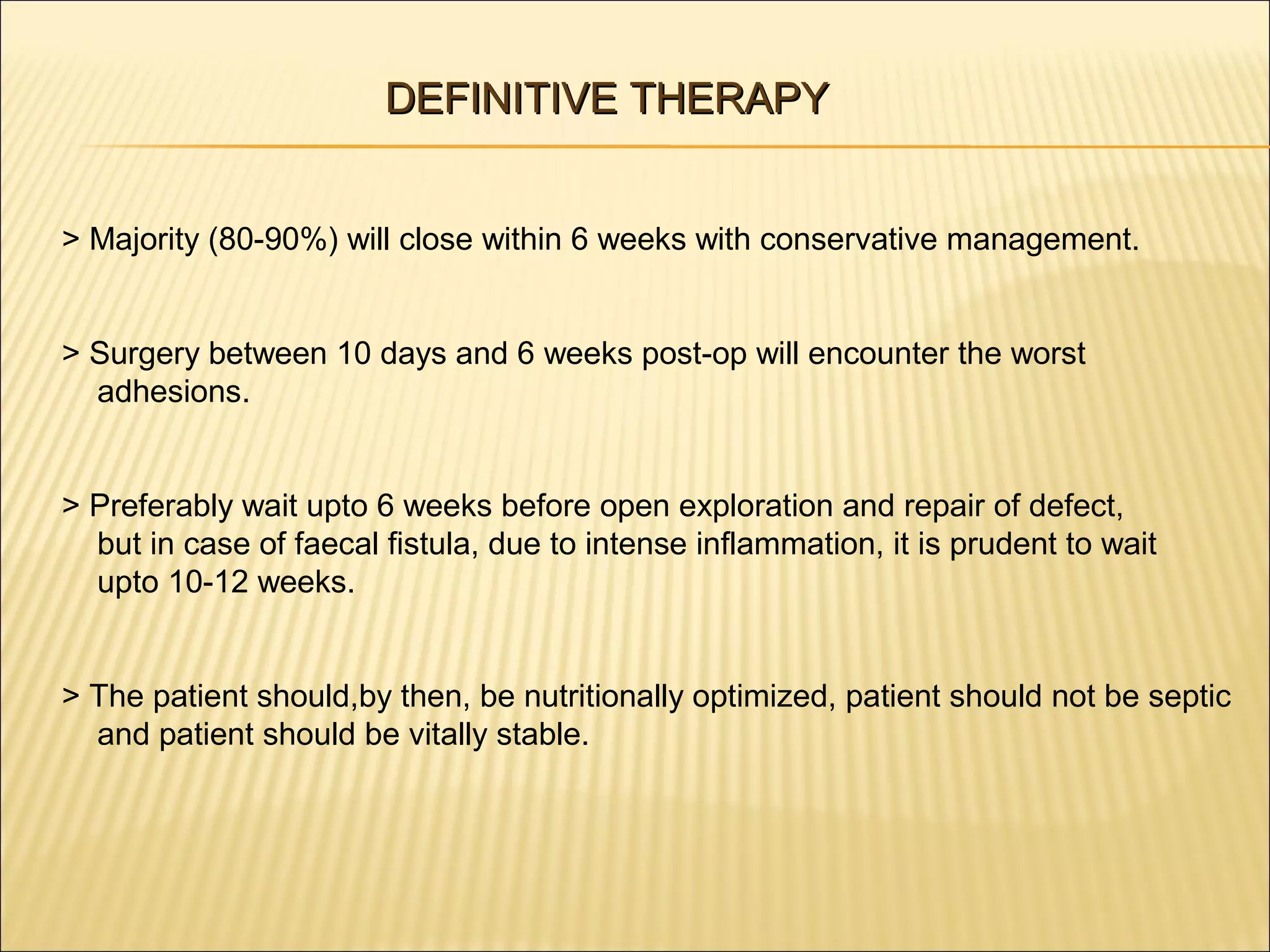
![NUTRITION CONTD..
TYPE OF FISTULA
CALORIE REQ
PROTEIN REQ
Low Output
30-35 kcal/kg/day
1-2 gm/kg/day
High Output
45-50 kcal/kg/day
1.5-2.5 gm/kg/day
> Twice the daily requirement of vitamins, trace elements, zinc and upto 10 times
the daily requirement of Vitamin C should be provided.
> Short turnover proteins like retinol-binding protein, prealbumin, ferritin can be
used to monitor the weekly efficacy of protein delivery. [Alb half life is 20 days].
> Mortality rate of 42% with alb <2.5 mg/dl vs 0% if >3.5 mg/dl.](https://image.slidesharecdn.com/enterocutaneous-fistulasppt-131126215812-phpapp02/75/Enterocutaneous-fistulas-ppt-17-2048.jpg)

![C. CONTROL OF SEPSIS AND FISTULA EFFLUENT CONTD..
> Vacuum assisted closure [VAC] device drainage system maybe used too.
> Due to the negative pressure application, VAC device helps to control drainage,
minimizes the size of the abdominal wound, reduces frequency of dressing
and protects the skin while helping to promote fistula healing.
> For majority of ECFs, VAC devices have become the method of choice for
controlling fistula drainage and skin protection.](https://image.slidesharecdn.com/enterocutaneous-fistulasppt-131126215812-phpapp02/75/Enterocutaneous-fistulas-ppt-19-2048.jpg)






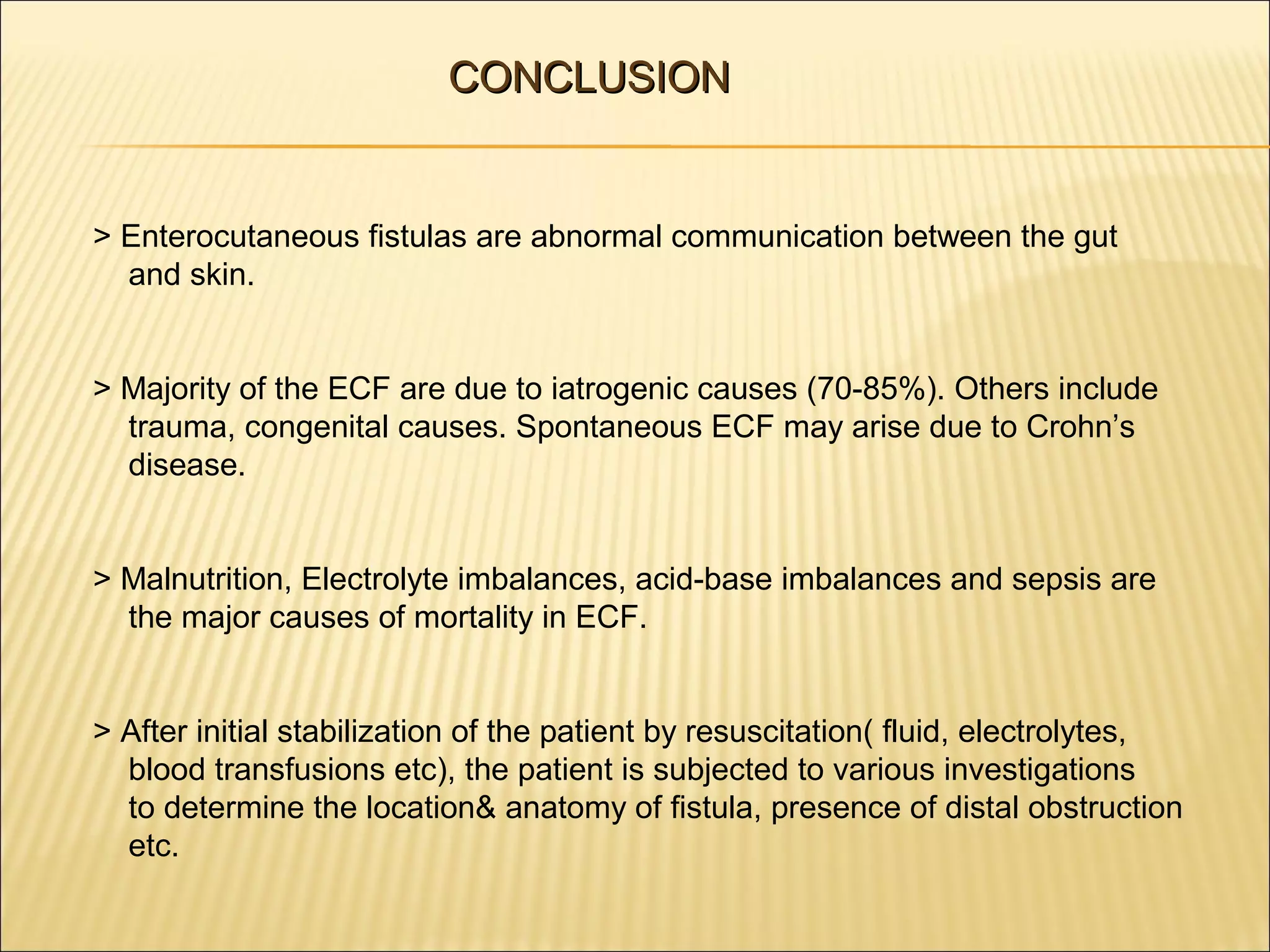
![> Reber et al reported that more than 90% of small intestinal fistula which
closed spontaneously,did so within a month.
> Spontaneous closure rates dropped to less than 10% after 2 months and
none after 3 months.
> Factors possibly responsible for failure of spontaneous closure are:
a. Foreign Body
b. Radiation
c. Inflammation/ infection
d. Epithelialisation
[F-R-I-E-N-D-S]
e. Neoplasm
f. Distal intestinal obstruction
g. Steroids.](https://image.slidesharecdn.com/enterocutaneous-fistulasppt-131126215812-phpapp02/75/Enterocutaneous-fistulas-ppt-28-2048.jpg)