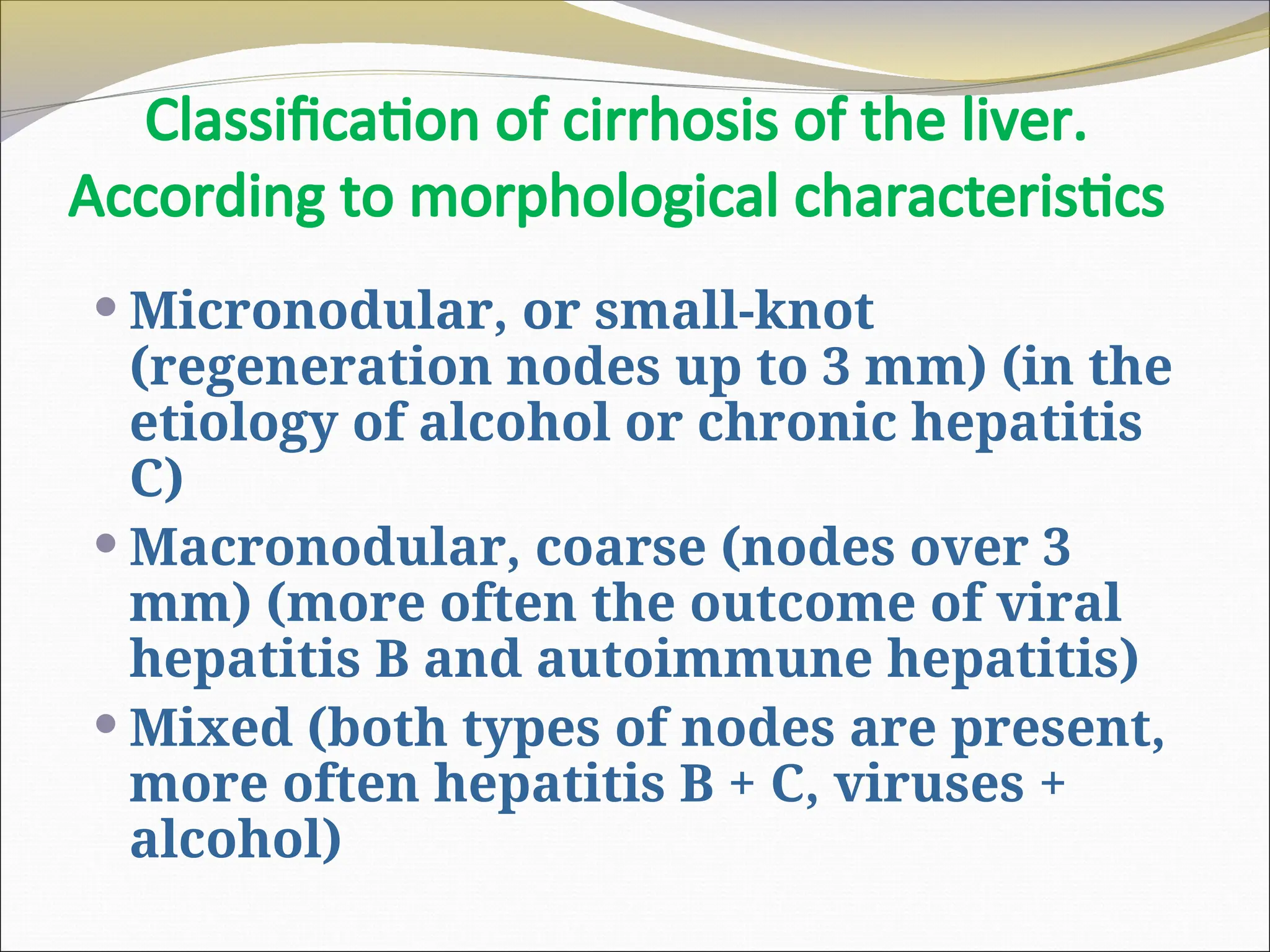
The document is a detailed lecture on liver cirrhosis, covering its anatomical, pathological, and clinical aspects, including definitions, etiologies (such as viral infections and alcohol), and classifications. It discusses the progression of the disease, diagnostic methods, and treatment options, emphasizing the complexity of managing cirrhosis and its complications. The document also includes prognostic factors based on the Child-Pugh scale, highlighting the varying life expectancy of patients depending on the severity of liver disease.