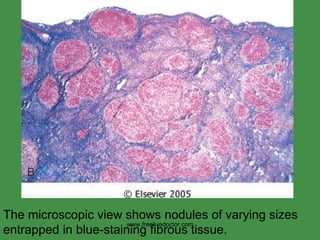
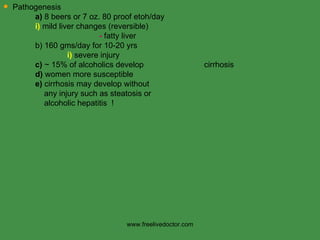
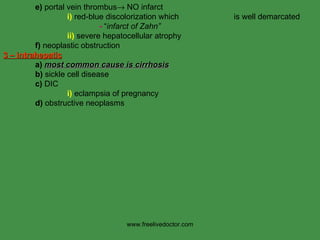
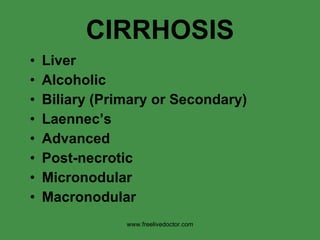
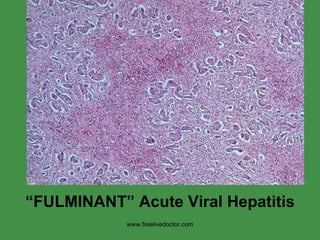
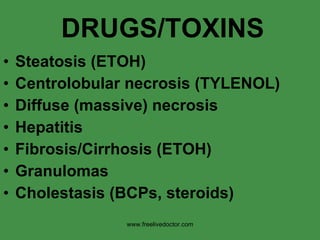
This document provides an overview of the liver and biliary tract anatomy and histology, as well as patterns of hepatic injury and disease. It describes the basic lobule structure of the liver and locations of the portal triad and central veins. Common liver diseases are summarized, including viral hepatitis, alcoholic hepatitis, cirrhosis, and malignancies like hepatocellular carcinoma. Biliary structures, gallbladder diseases, and extrahepatic considerations are also briefly covered.










































































![MAIN CONSIDERATIONS Anomalies Stones (Clolesterol/Bilirubin) (Chole[docho]lithiasis) Inflammation (Cholecystitis/Cholangitis) Cysts Neoplasms www.freelivedoctor.com](https://image.slidesharecdn.com/liverpothology-100416234842-phpapp02/85/Liver-pothology-79-320.jpg)