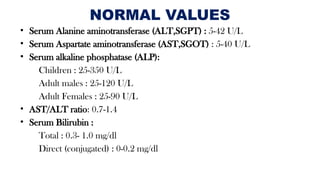
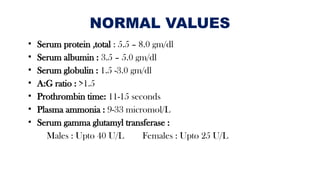
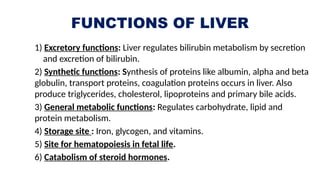
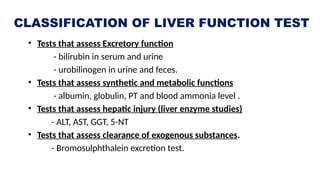
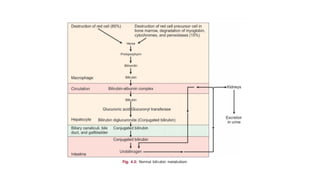
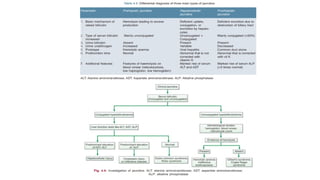
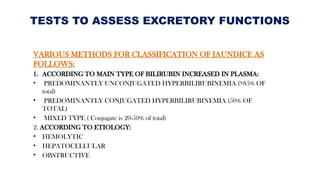
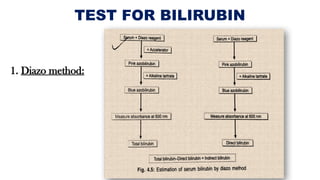
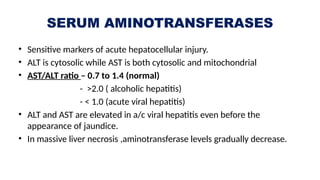
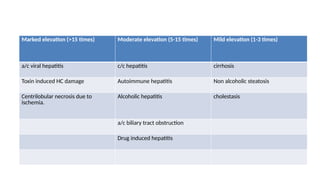
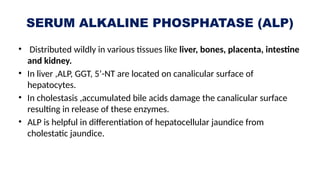
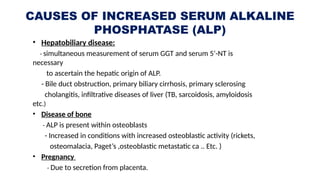
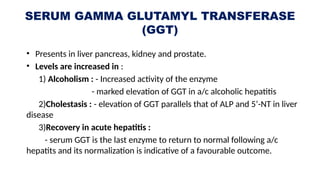
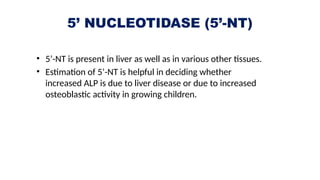
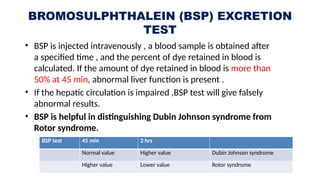
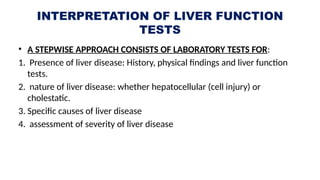
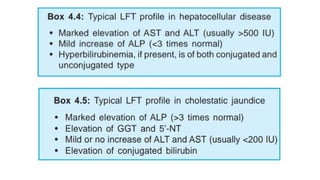
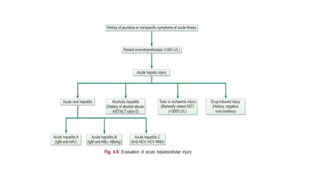
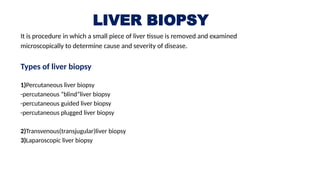
The document provides an overview of liver function tests, including normal values for various liver enzymes, proteins, and bilirubin. It outlines the liver's functions such as excretion, synthesis, storage, and metabolism, as well as the classifications of liver function tests. It also discusses the assessment of liver injuries and describes the methodology and implications of various biopsy techniques.