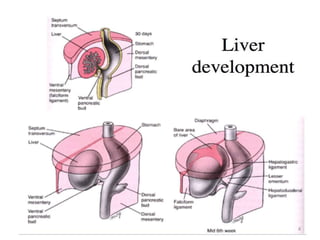
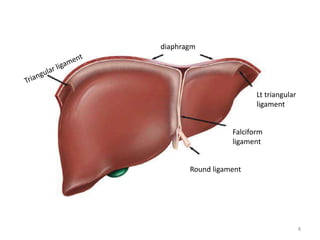
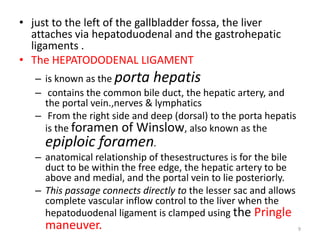
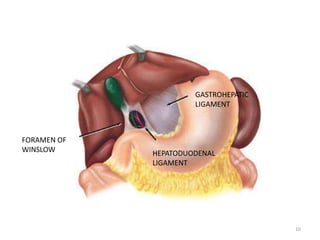
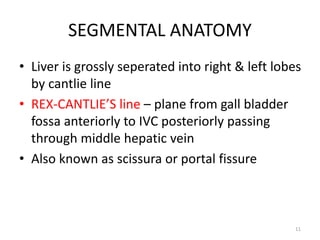
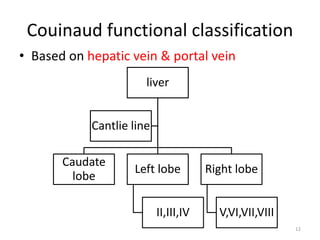
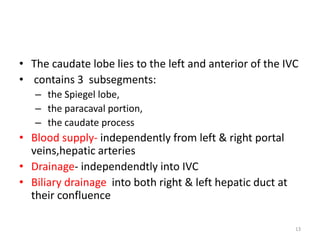
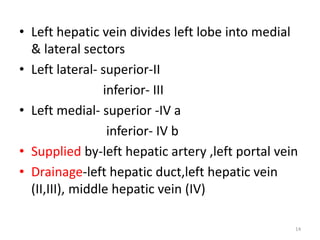
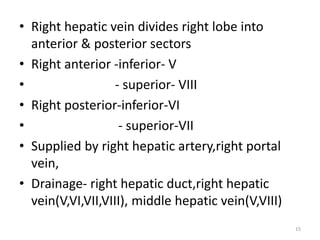
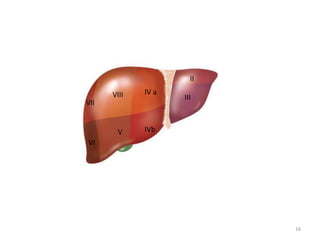
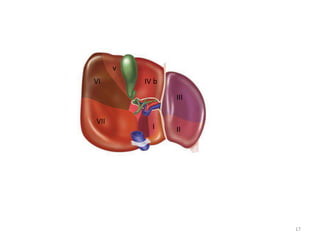
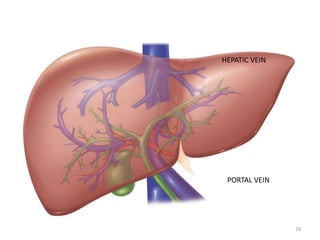
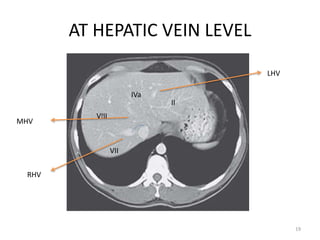
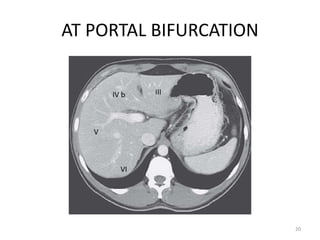
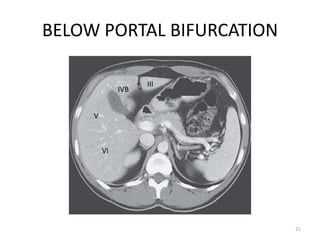
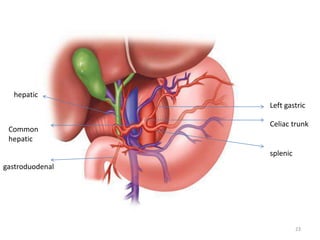
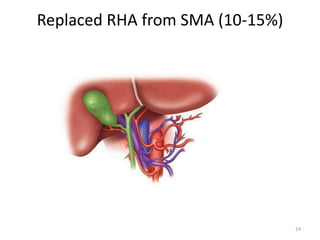
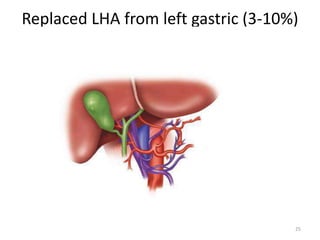
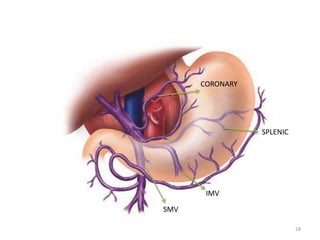
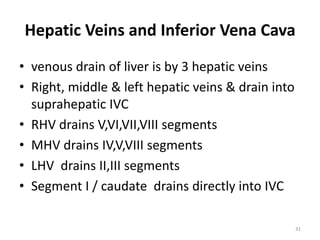
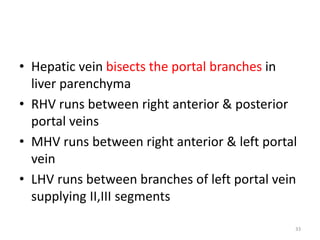
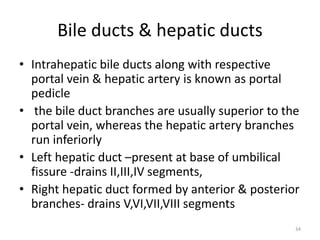
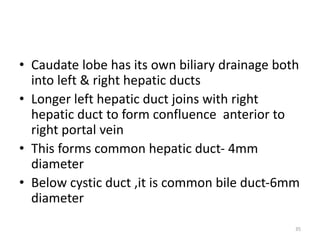
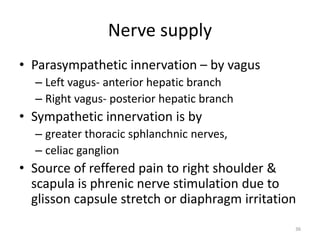
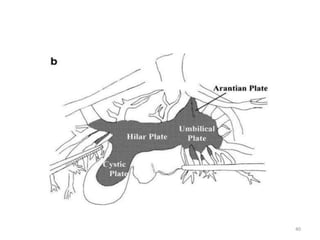
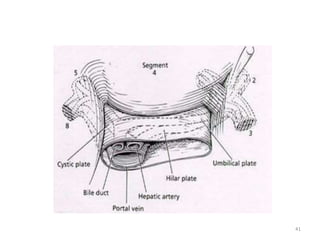
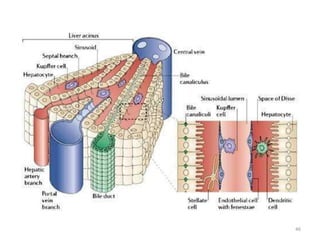
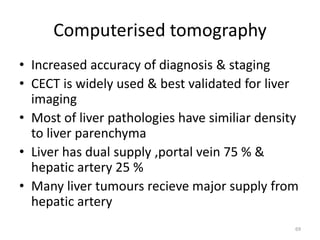
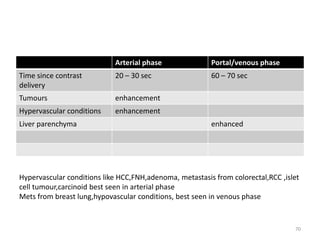
This document discusses liver anatomy, function tests, and imaging. It covers the embryological development of the liver, its lobes and ligament attachments. It describes the dual blood supply, biliary drainage system, and microscopic anatomy. Common liver function tests are outlined including those assessing synthesis, damage, and detoxification. Ultrasound imaging of the liver is also summarized, noting its advantages of being inexpensive and non-invasive but limitations in imaging certain areas.