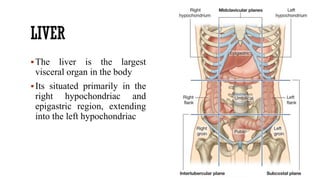
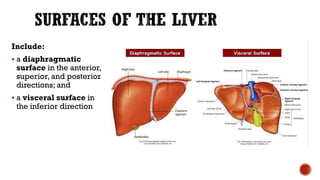
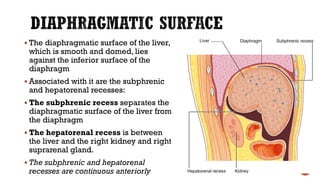
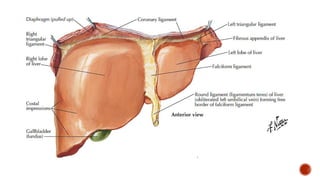
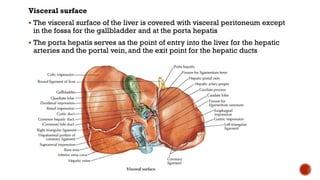
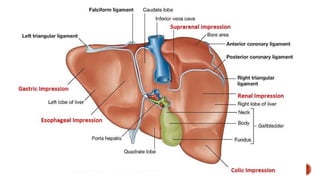
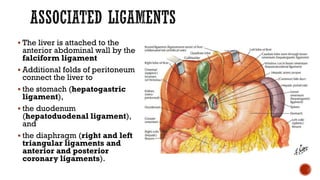
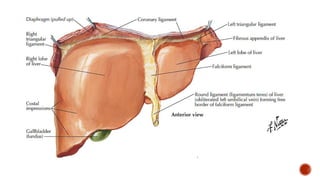
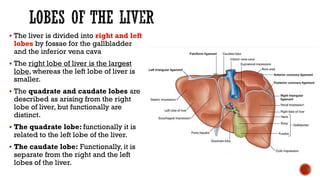
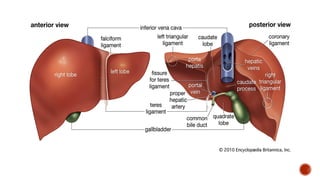
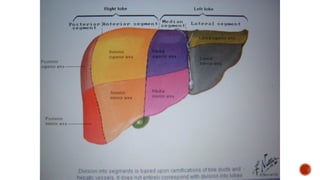
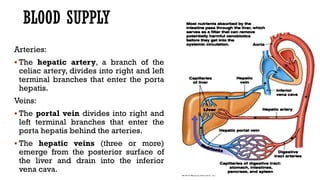
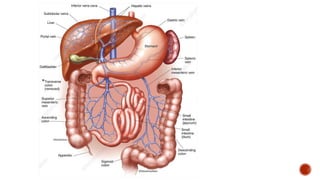
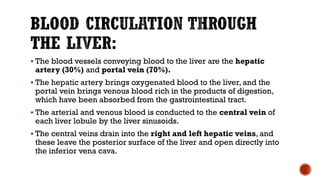
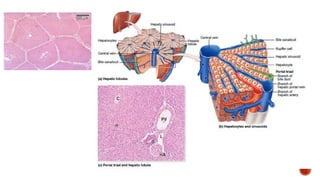
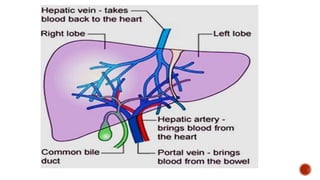
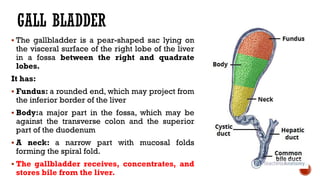
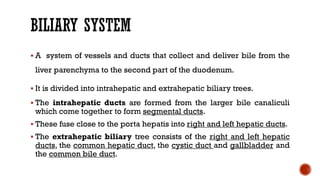
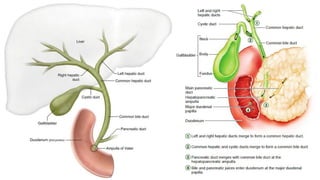
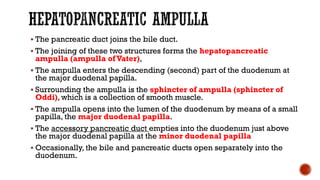
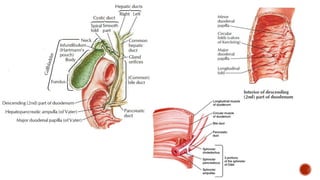
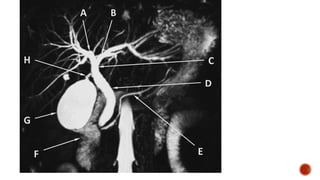
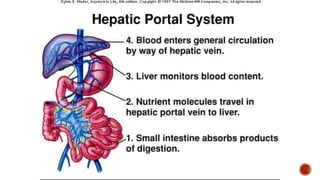
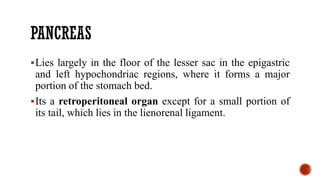
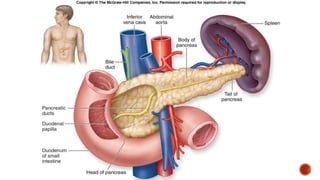
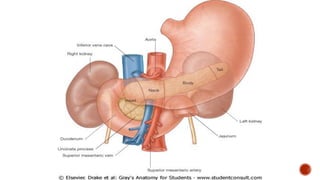
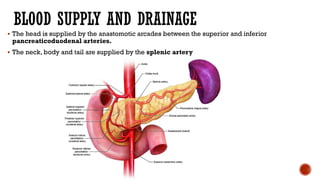
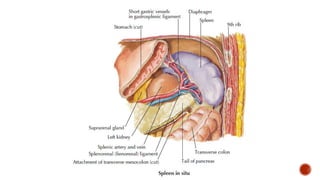
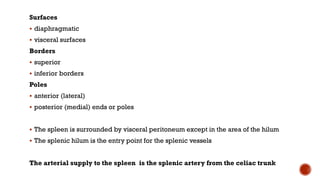
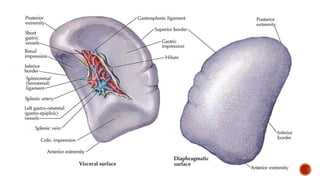
The liver is the largest visceral organ, playing key roles in bile production, detoxification, and storage of nutrients. It develops from the hepatic diverticulum and is connected to various structures, including the gallbladder and pancreas, through a complex vascular and biliary system. Additionally, the spleen functions in hematopoiesis and is situated between the stomach and diaphragm, connected to surrounding structures by ligaments.