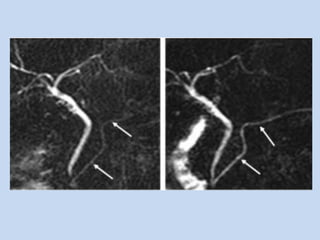
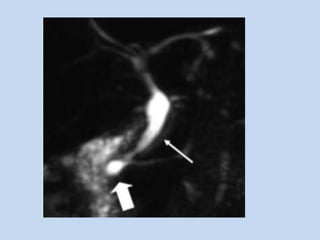
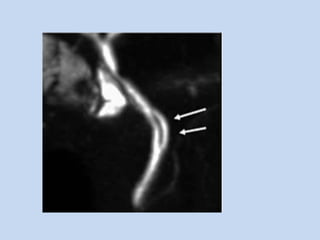
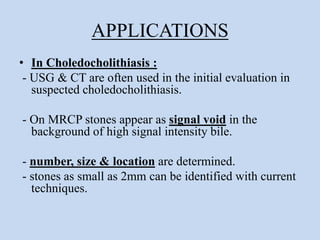
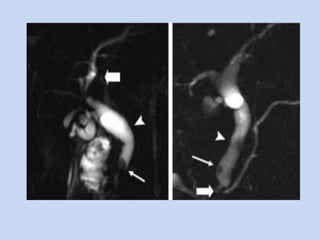
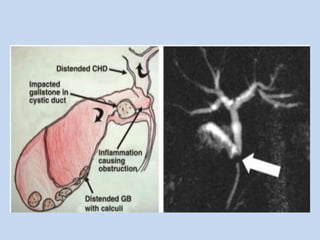
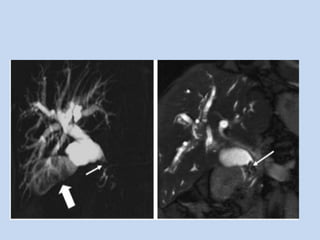
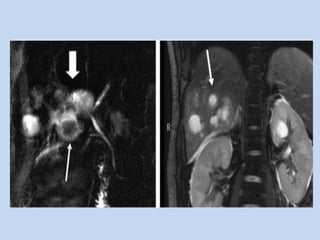
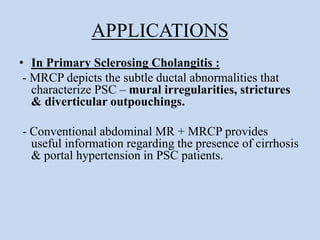
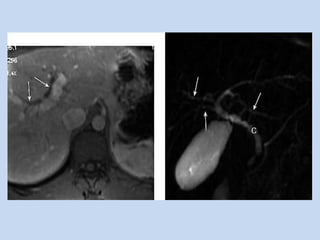
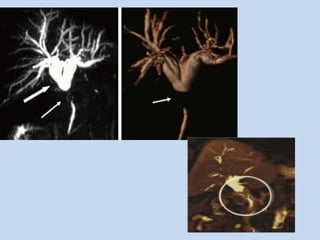
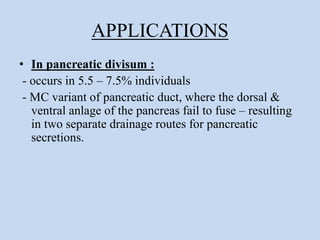
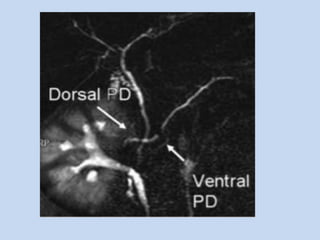
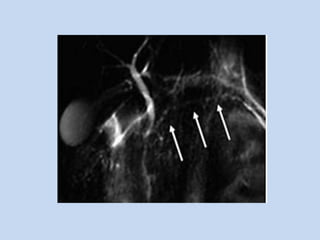
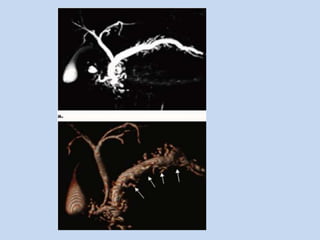
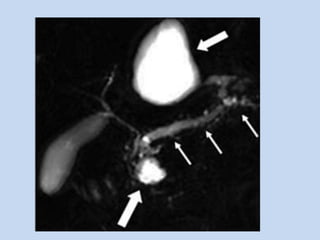
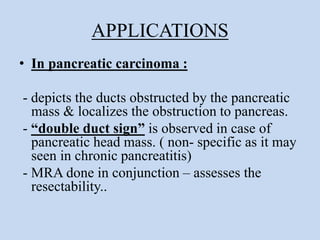
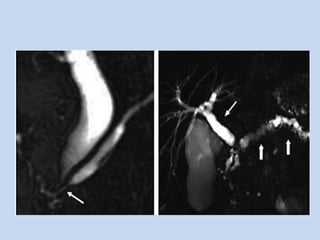
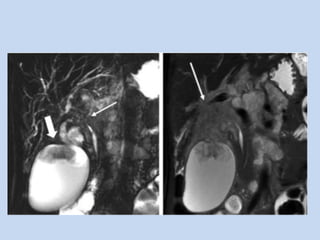
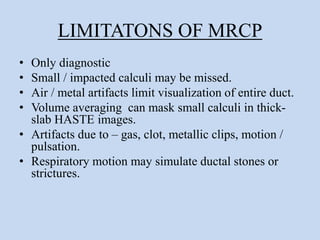
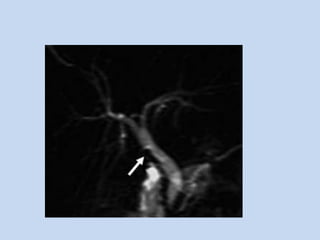
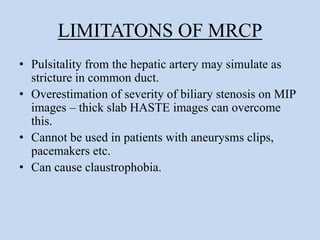
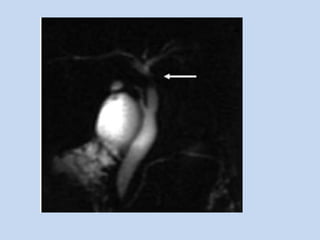
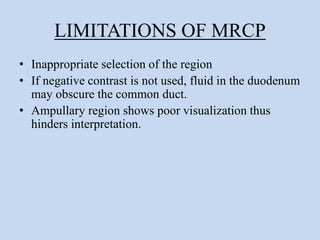
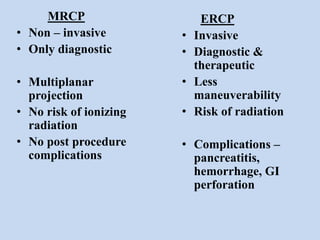
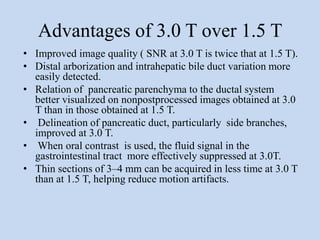
This document provides an overview of magnetic resonance cholangiopancreatography (MRCP). It discusses patient preparation, techniques, advantages, limitations, and clinical applications of MRCP. Key points include: MRCP uses heavily T2-weighted sequences to noninvasively visualize the biliary and pancreatic ducts. Patient preparation involves fasting and administering oral contrast. Thin-slab MRCP images provide high resolution of the ductal systems. MRCP is useful for evaluating biliary diseases, pancreatic diseases, and postoperative complications without radiation exposure. Limitations include inability to detect small stones and artifacts from gas or metal.