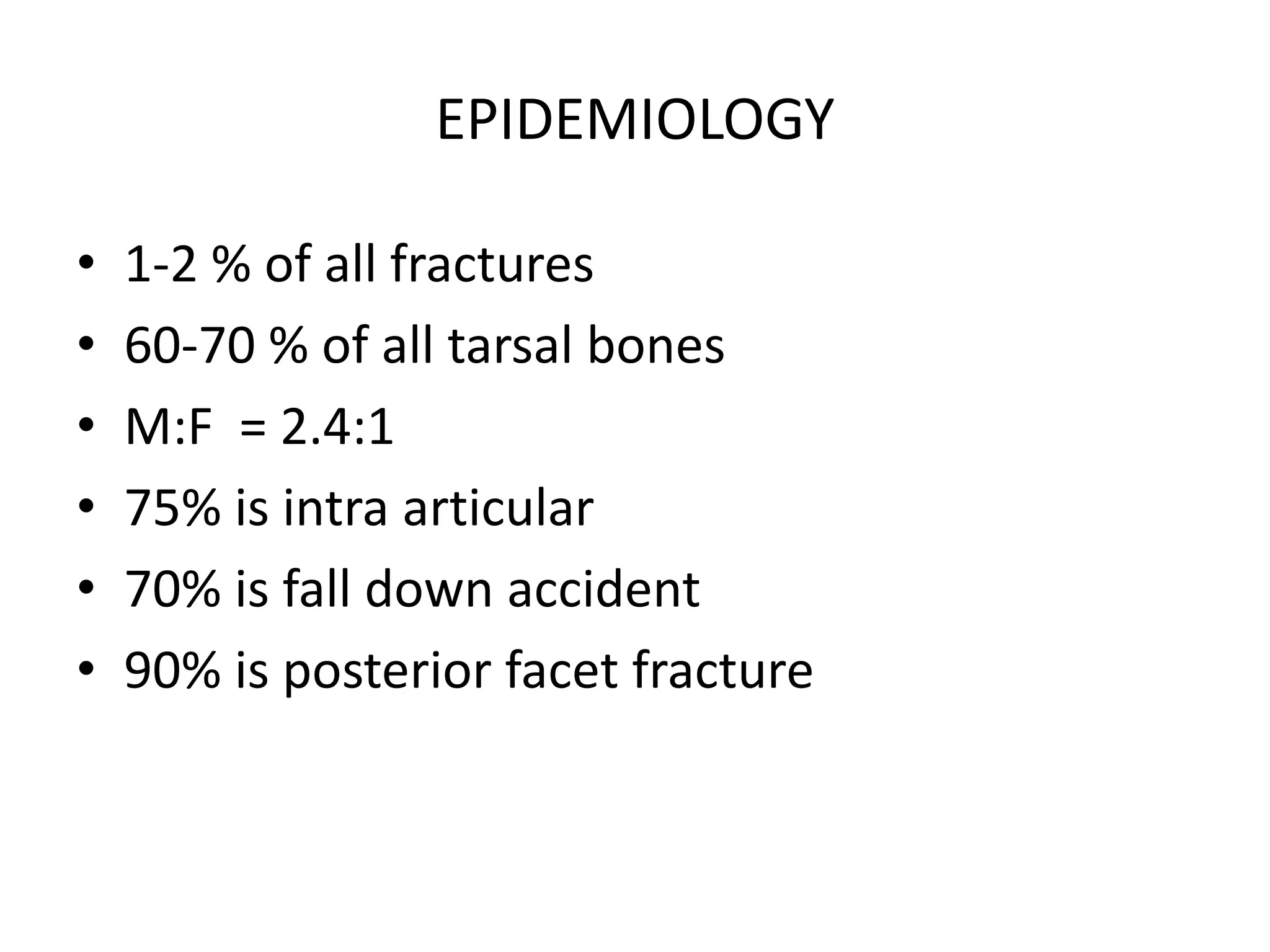
1) Talus and calcaneus fractures can result from high-energy injuries like falls or motor vehicle accidents.
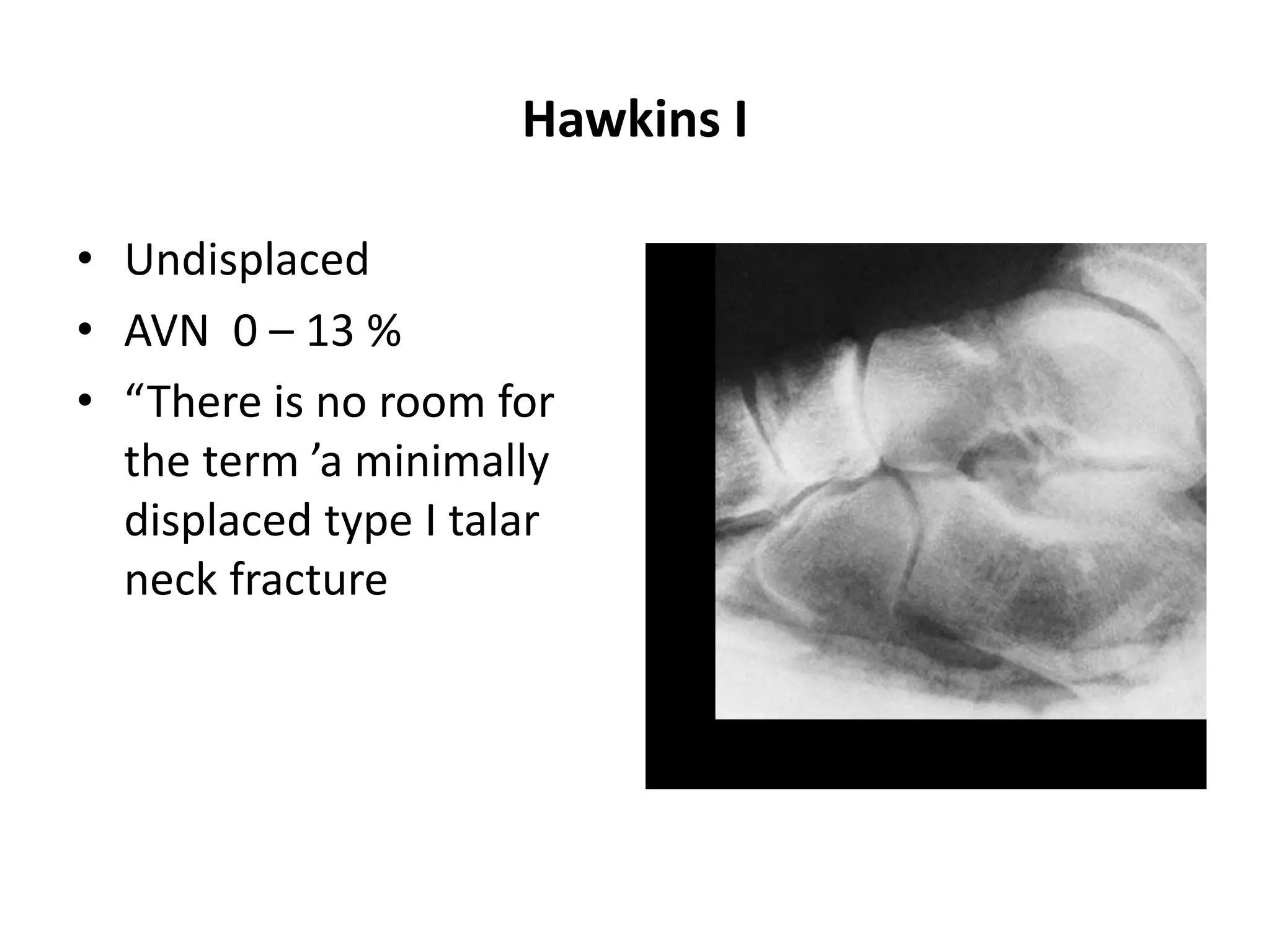
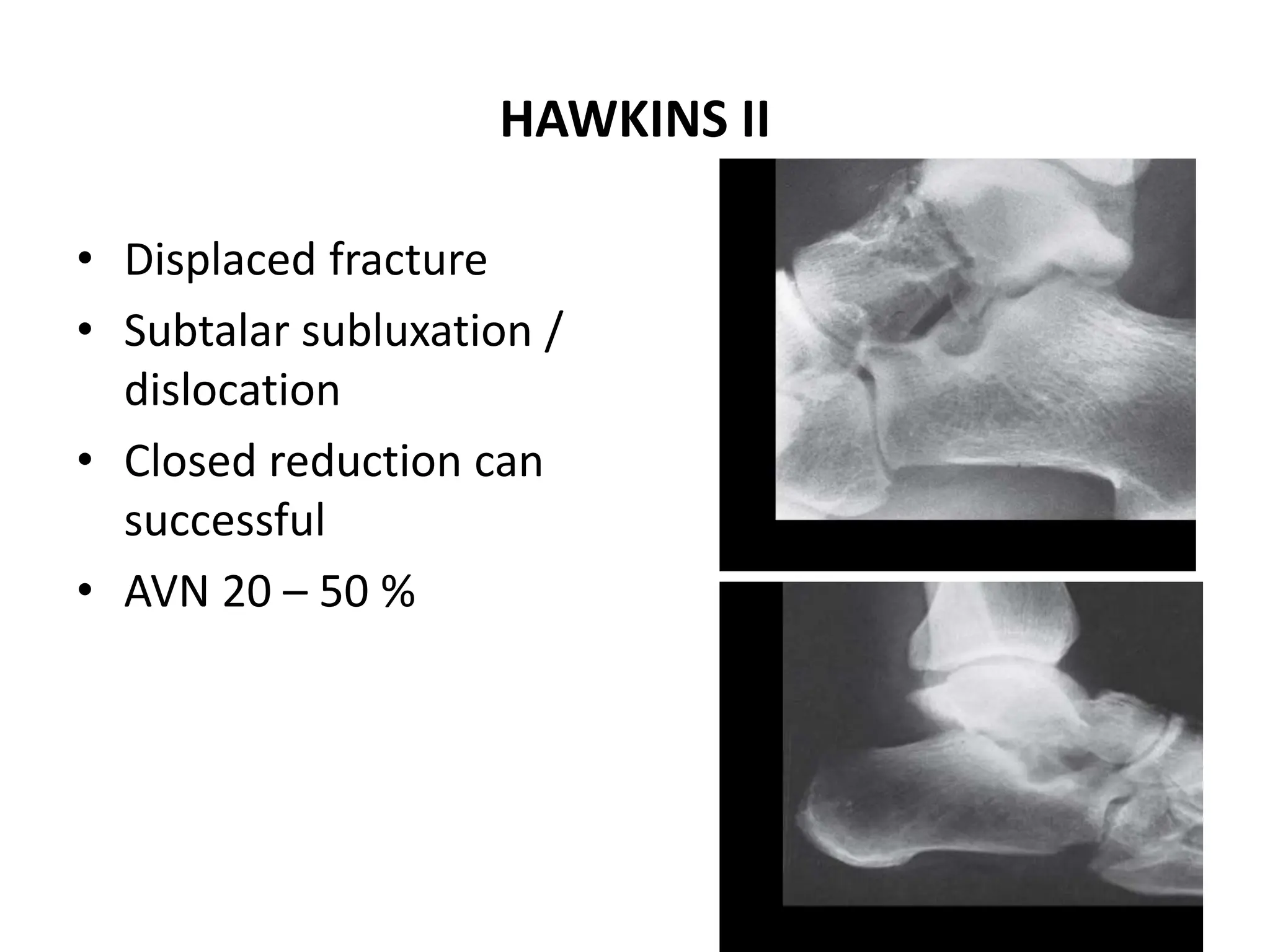
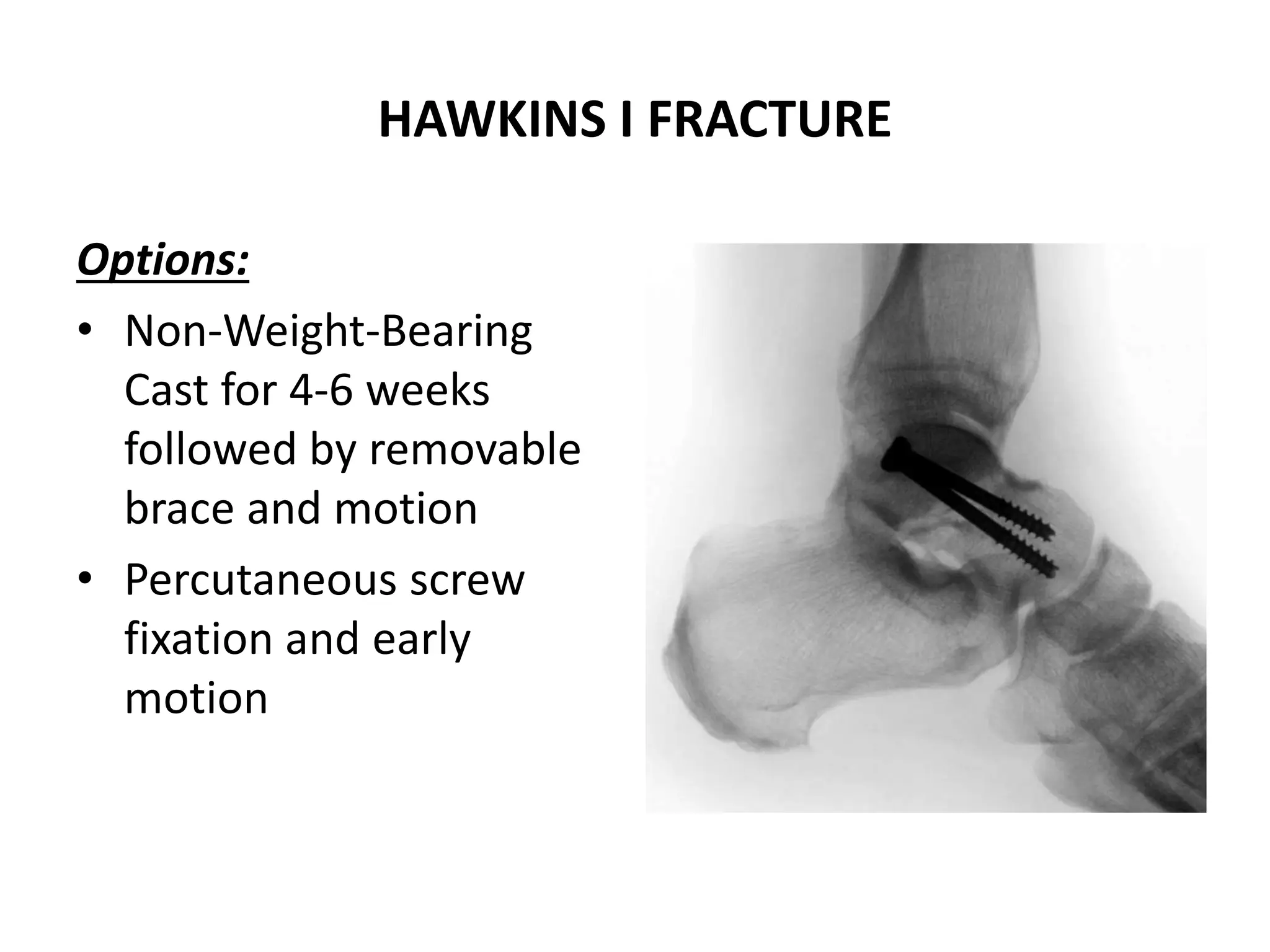
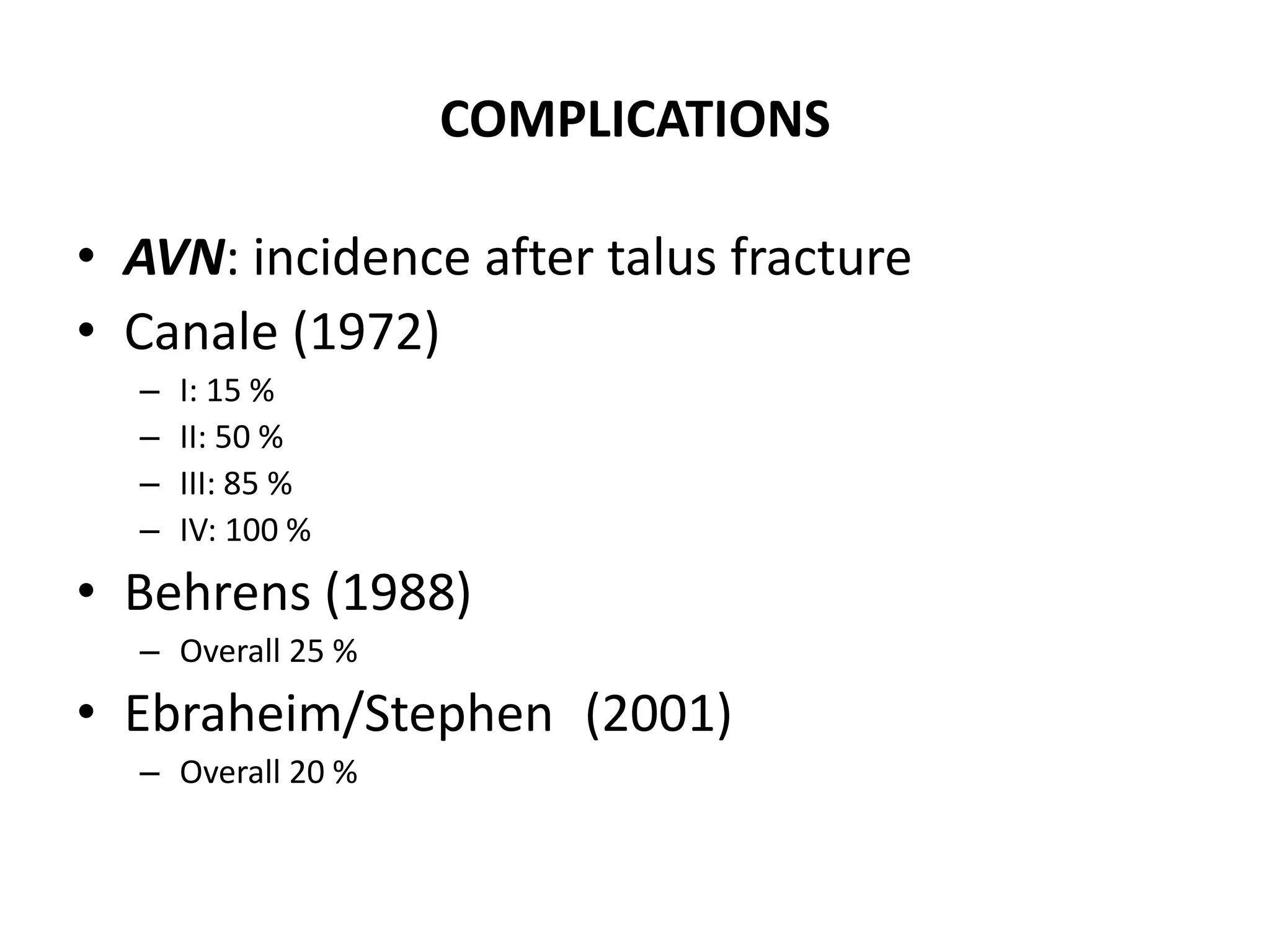
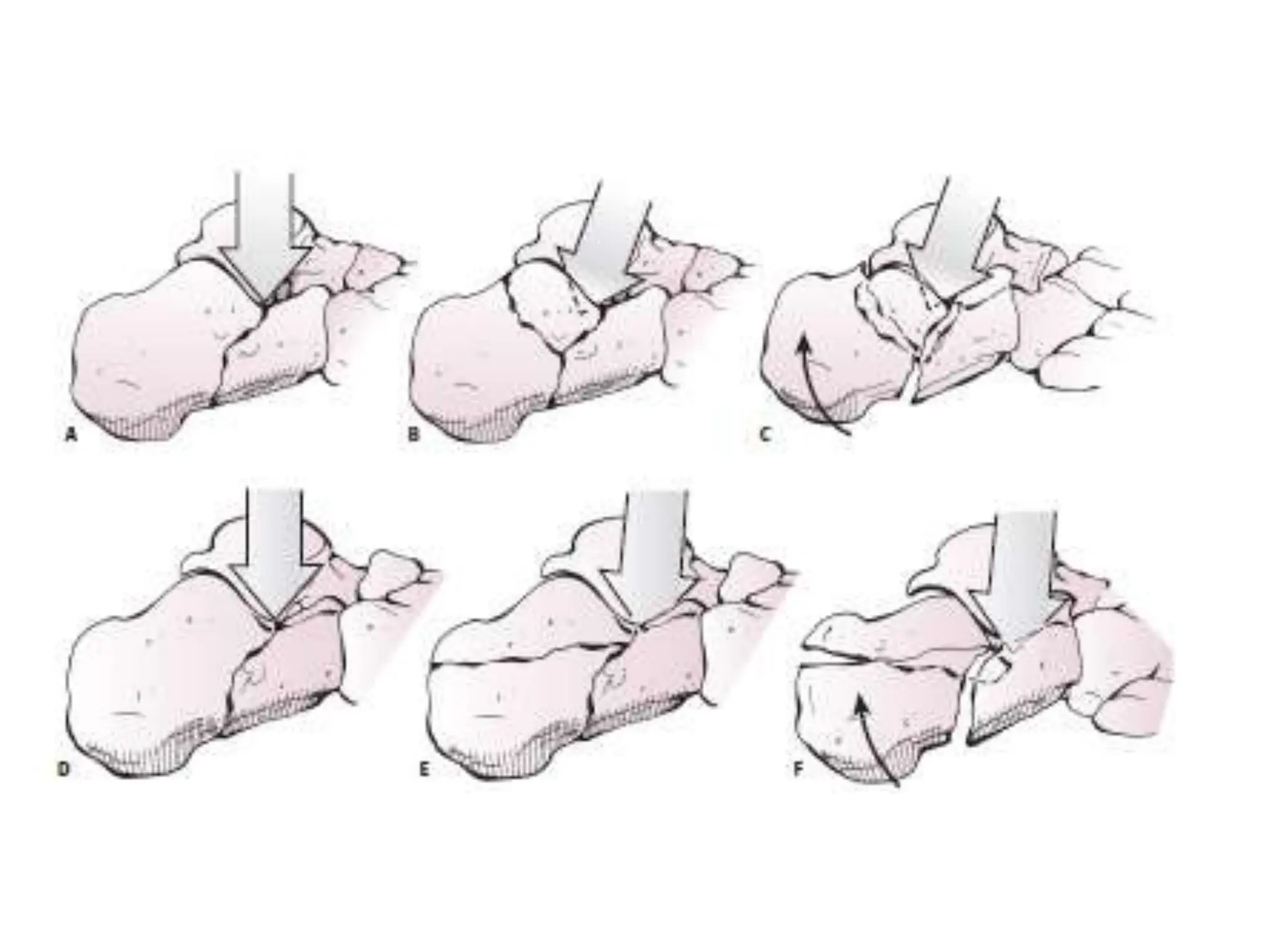
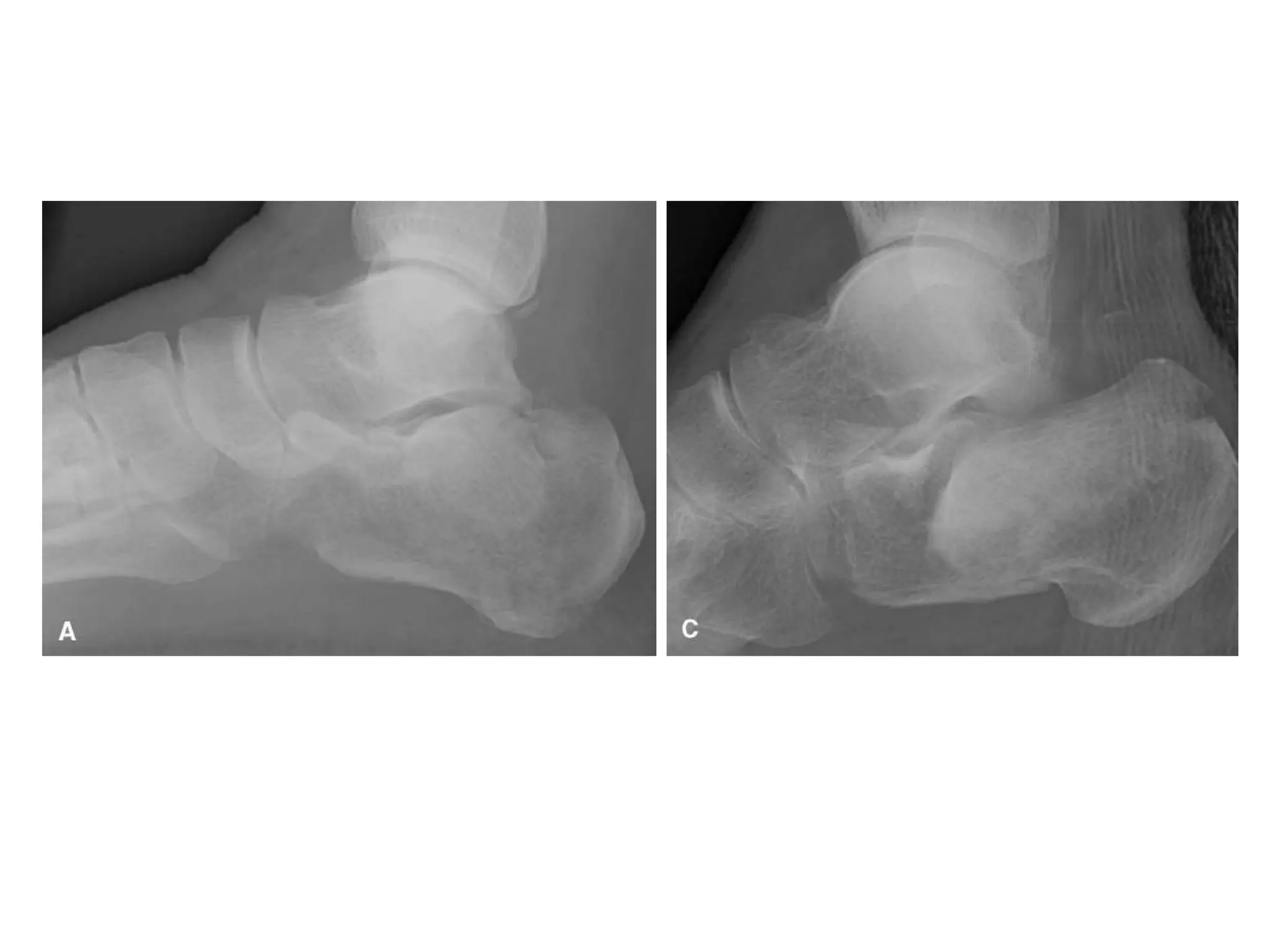
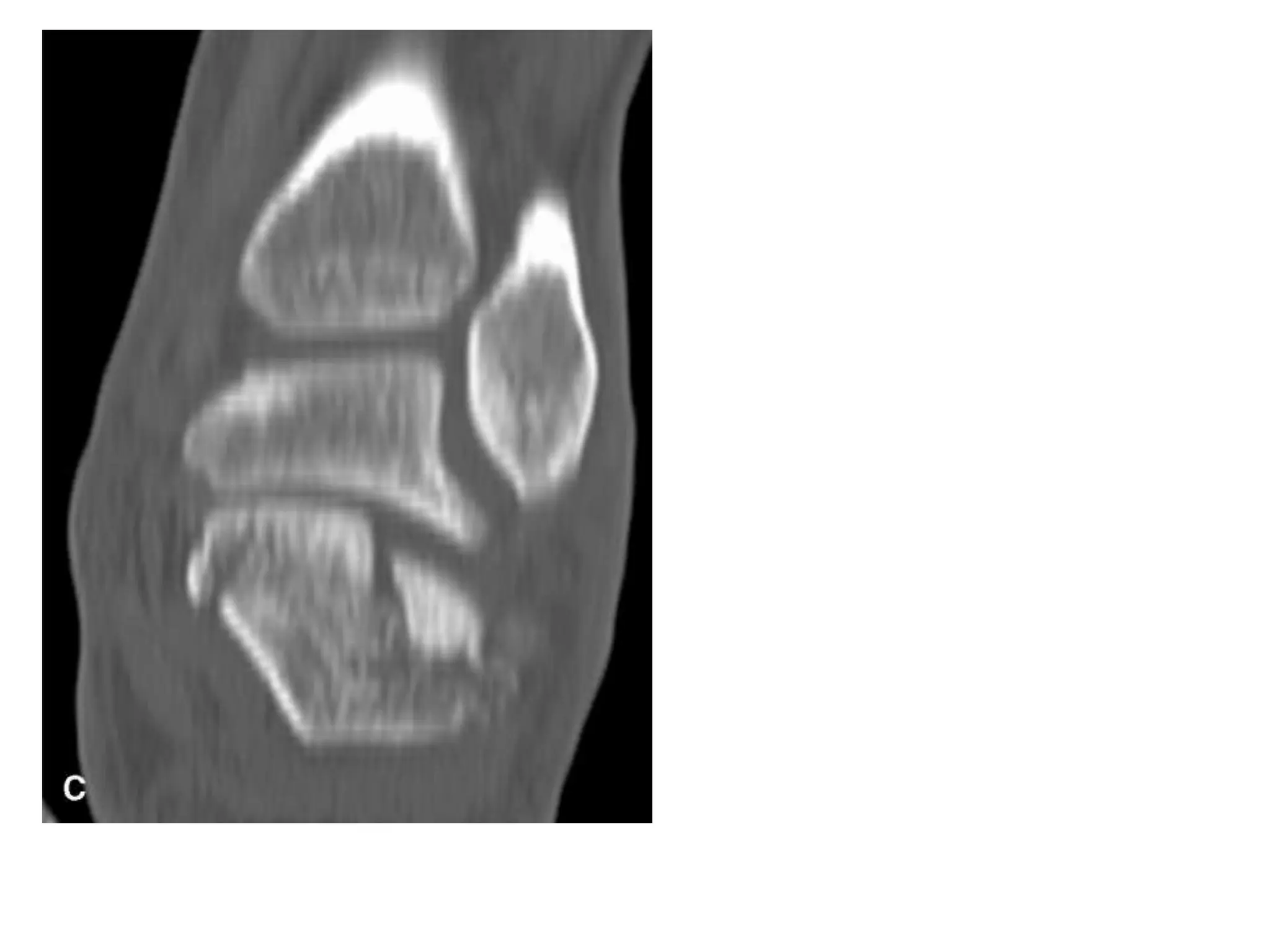
2) Hawkins classification is commonly used to describe talus neck fractures, with type I being undisplaced and having the lowest risk of avascular necrosis, while type III and IV involve dislocation and have the highest risk.
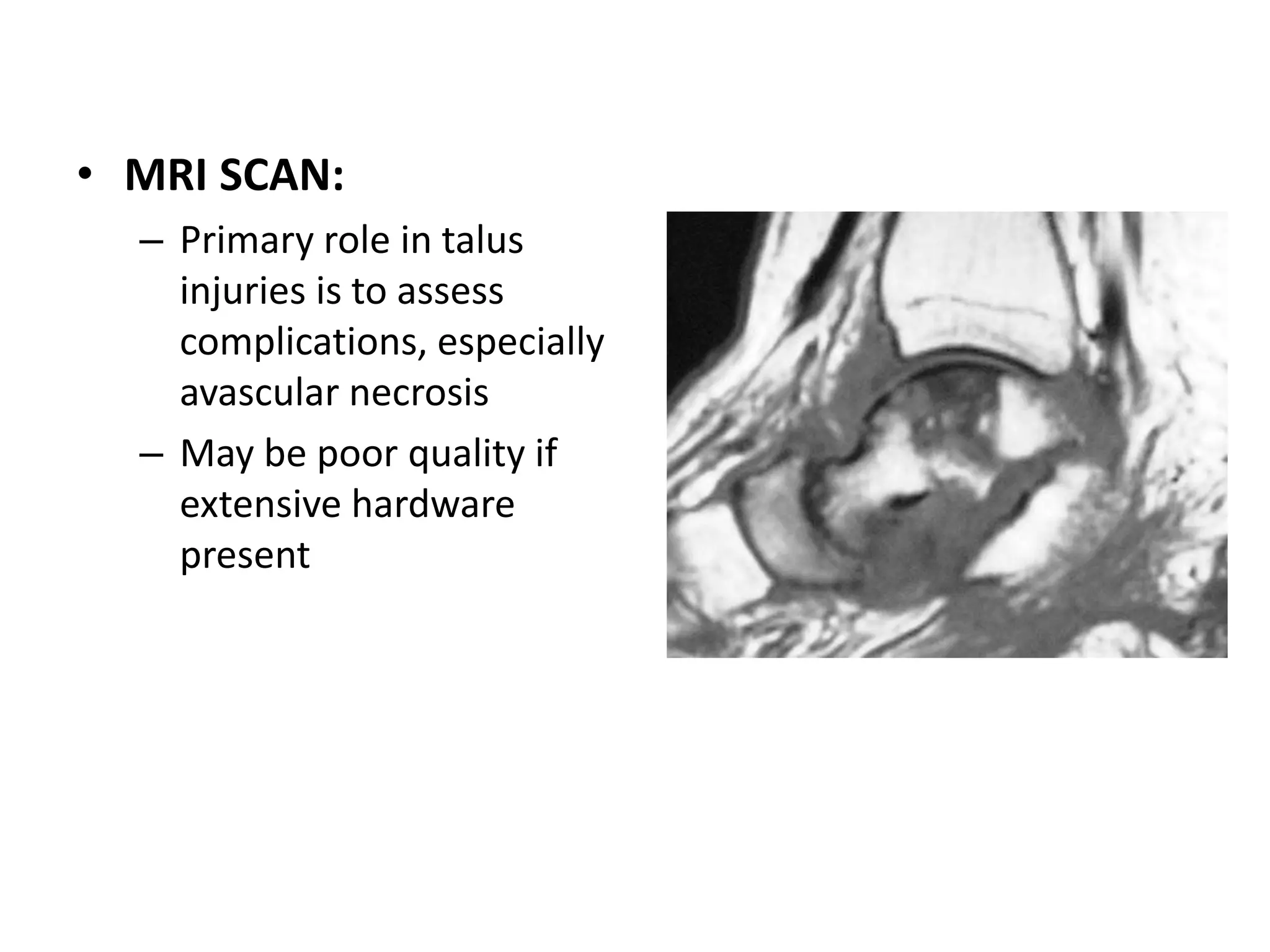
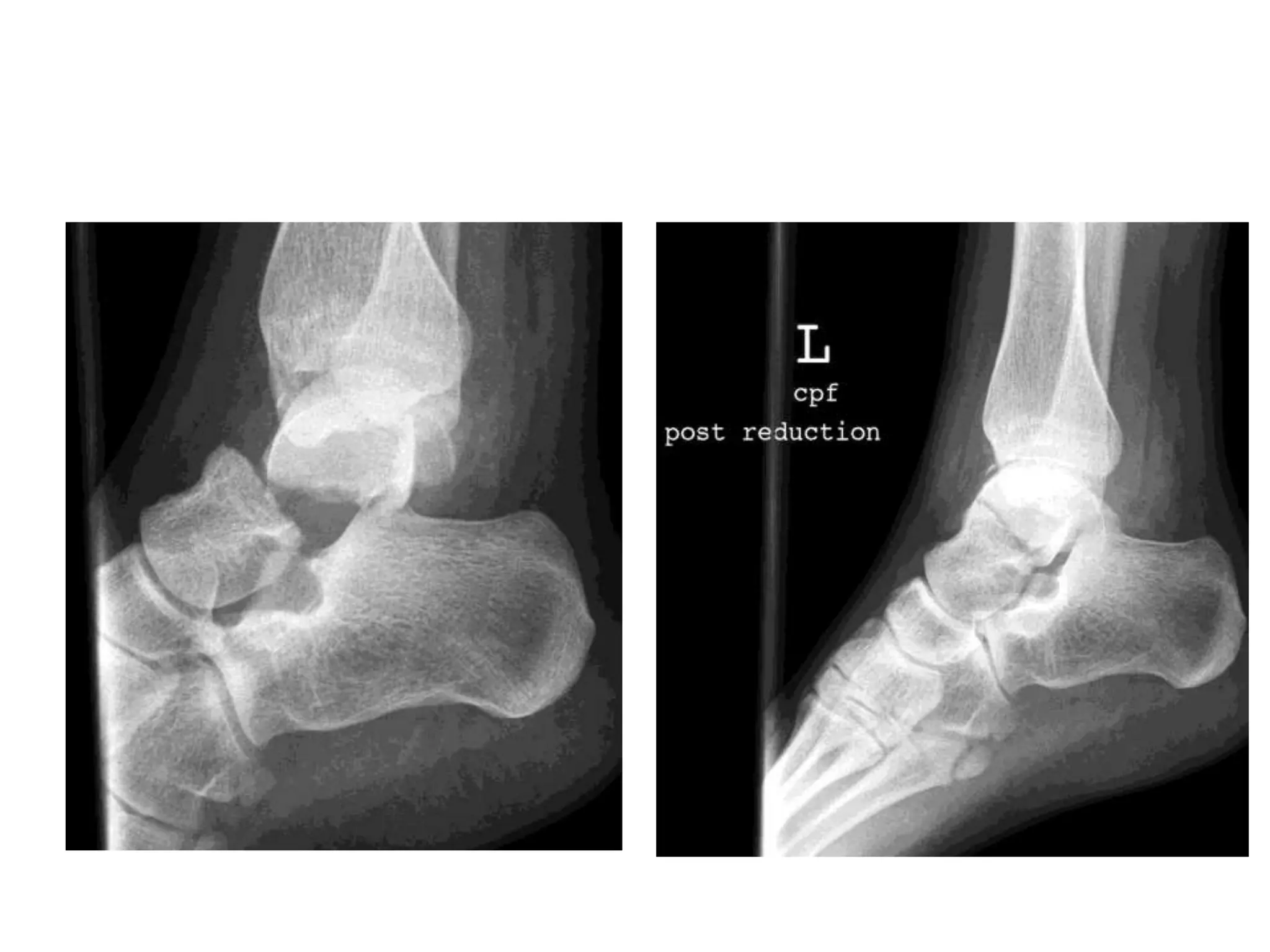
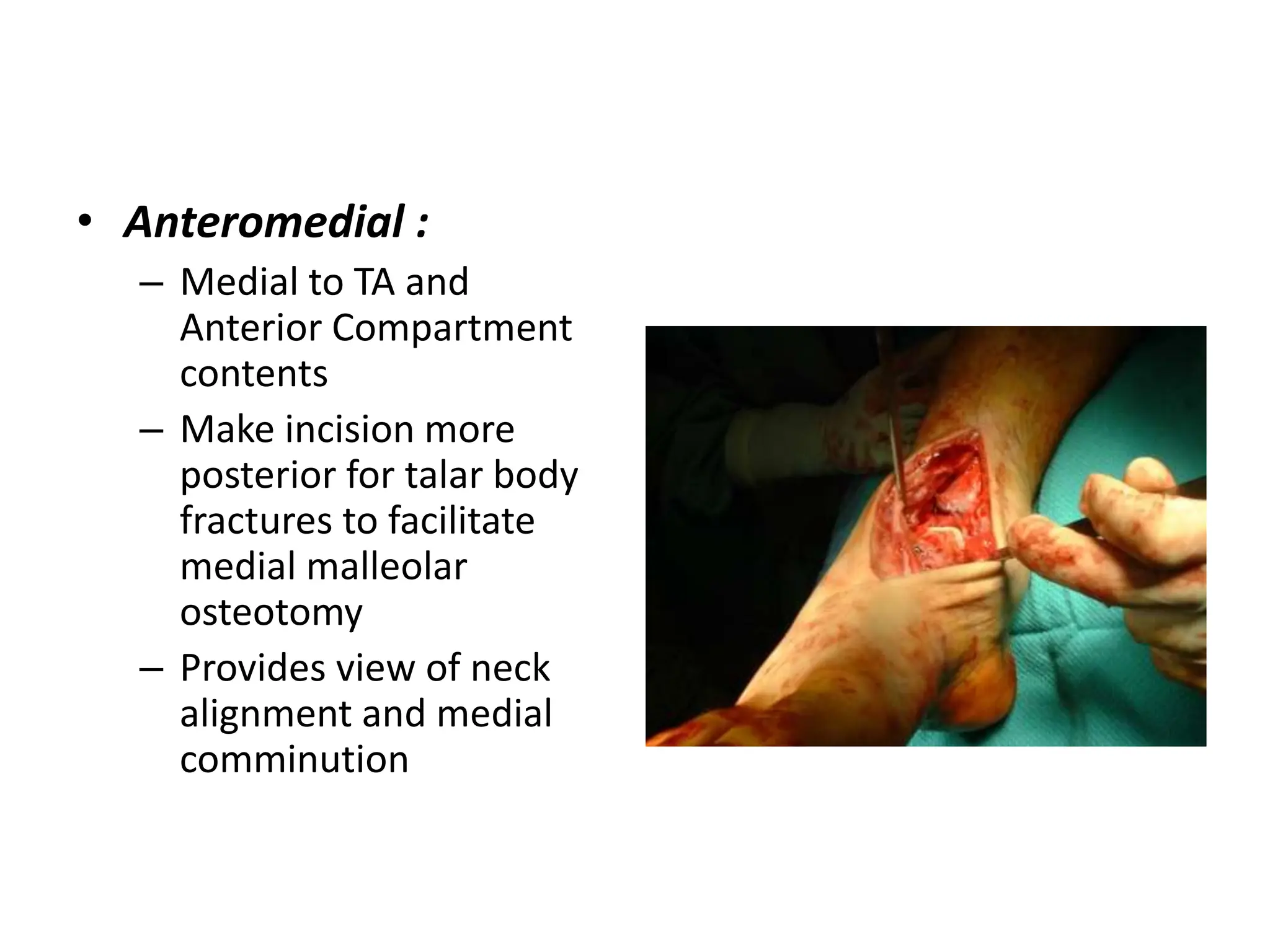
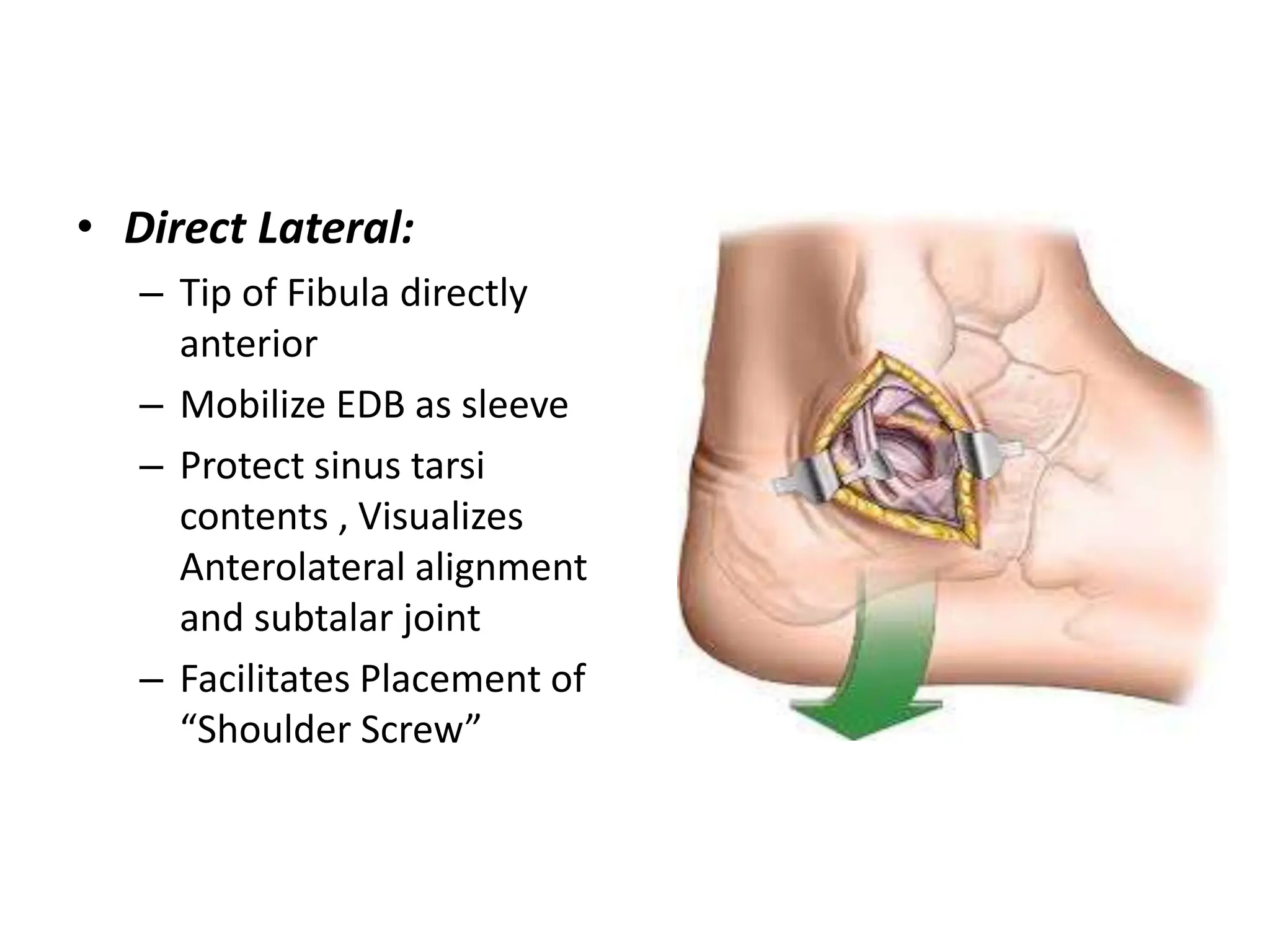
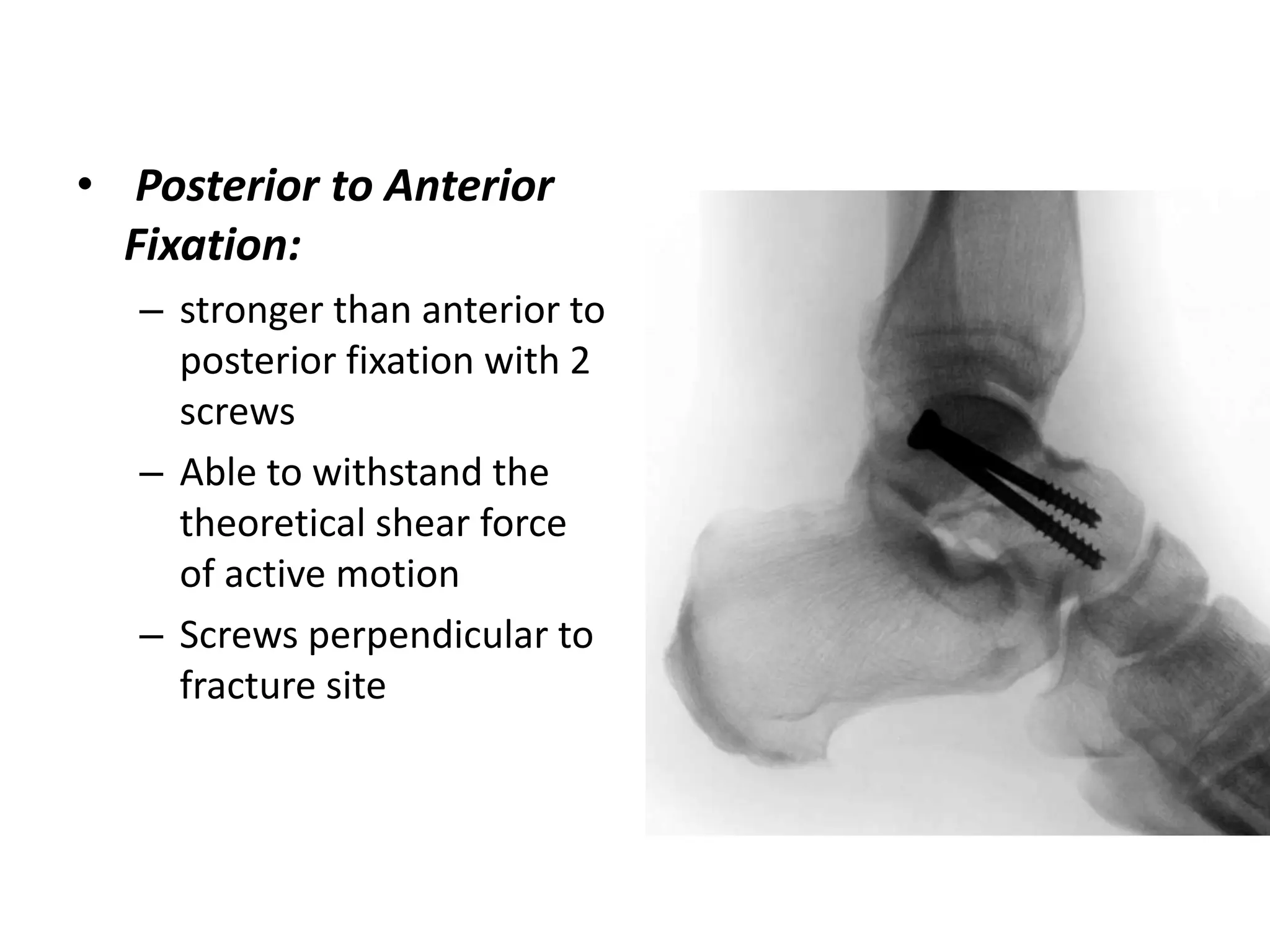
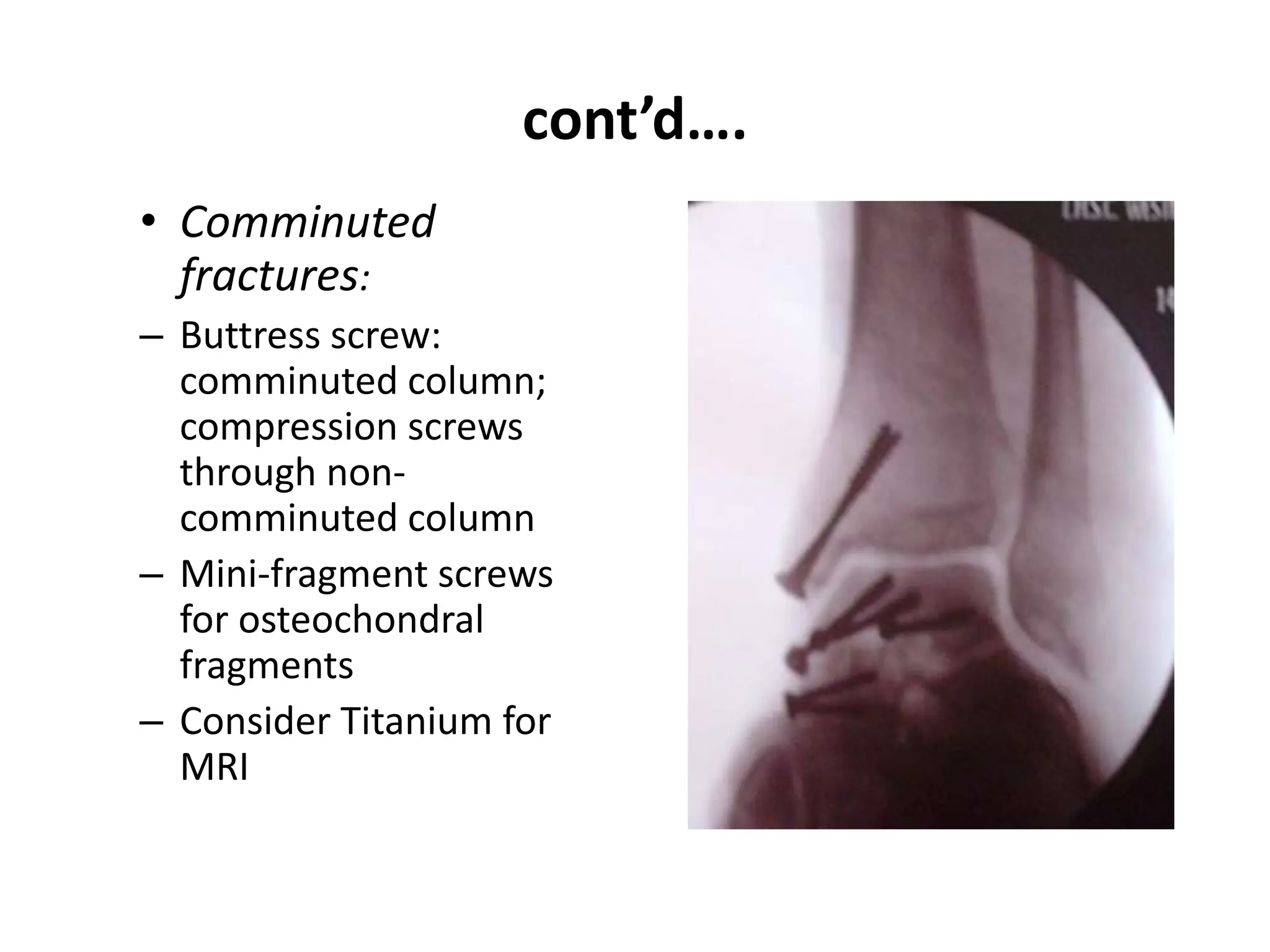
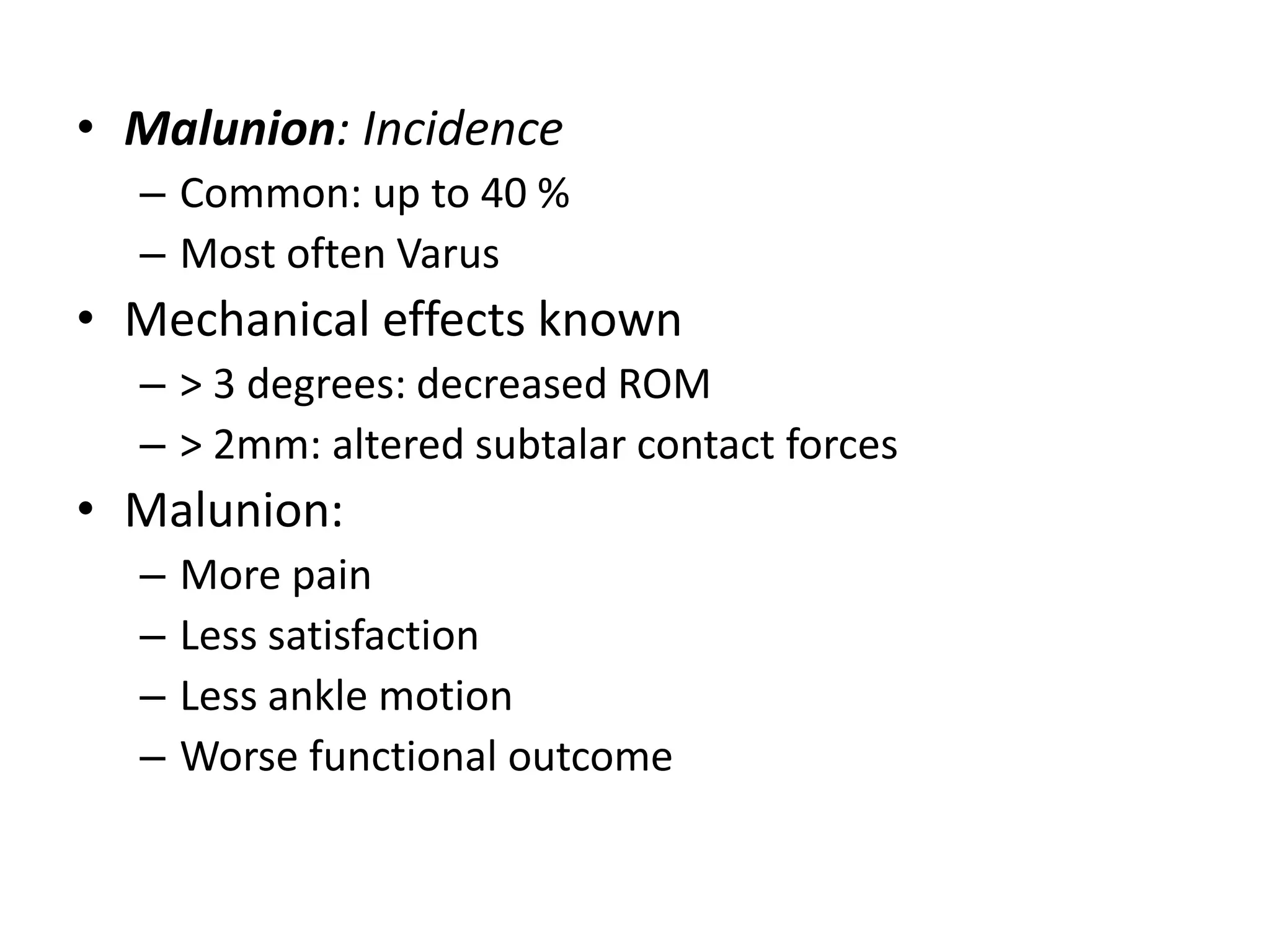
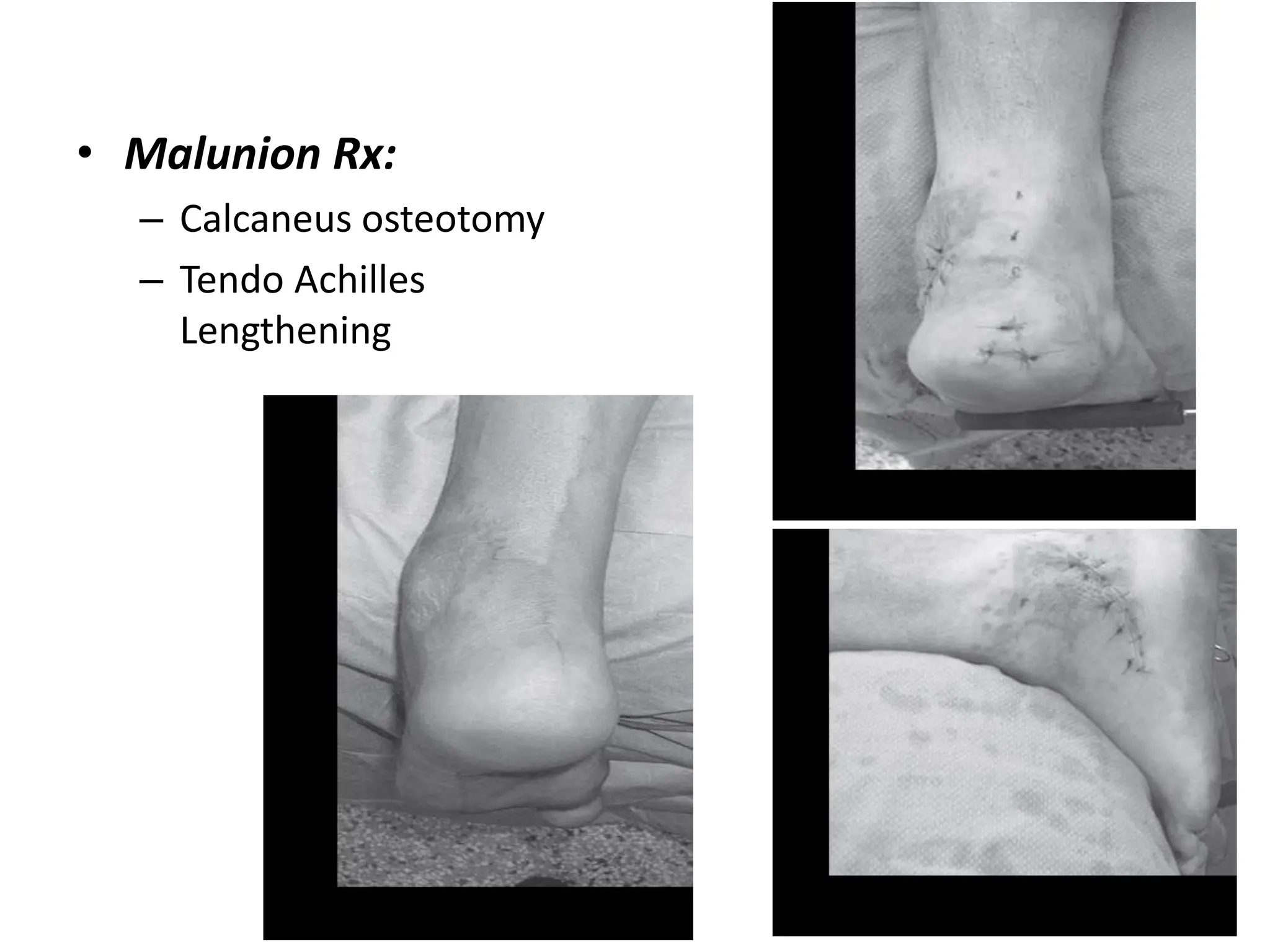
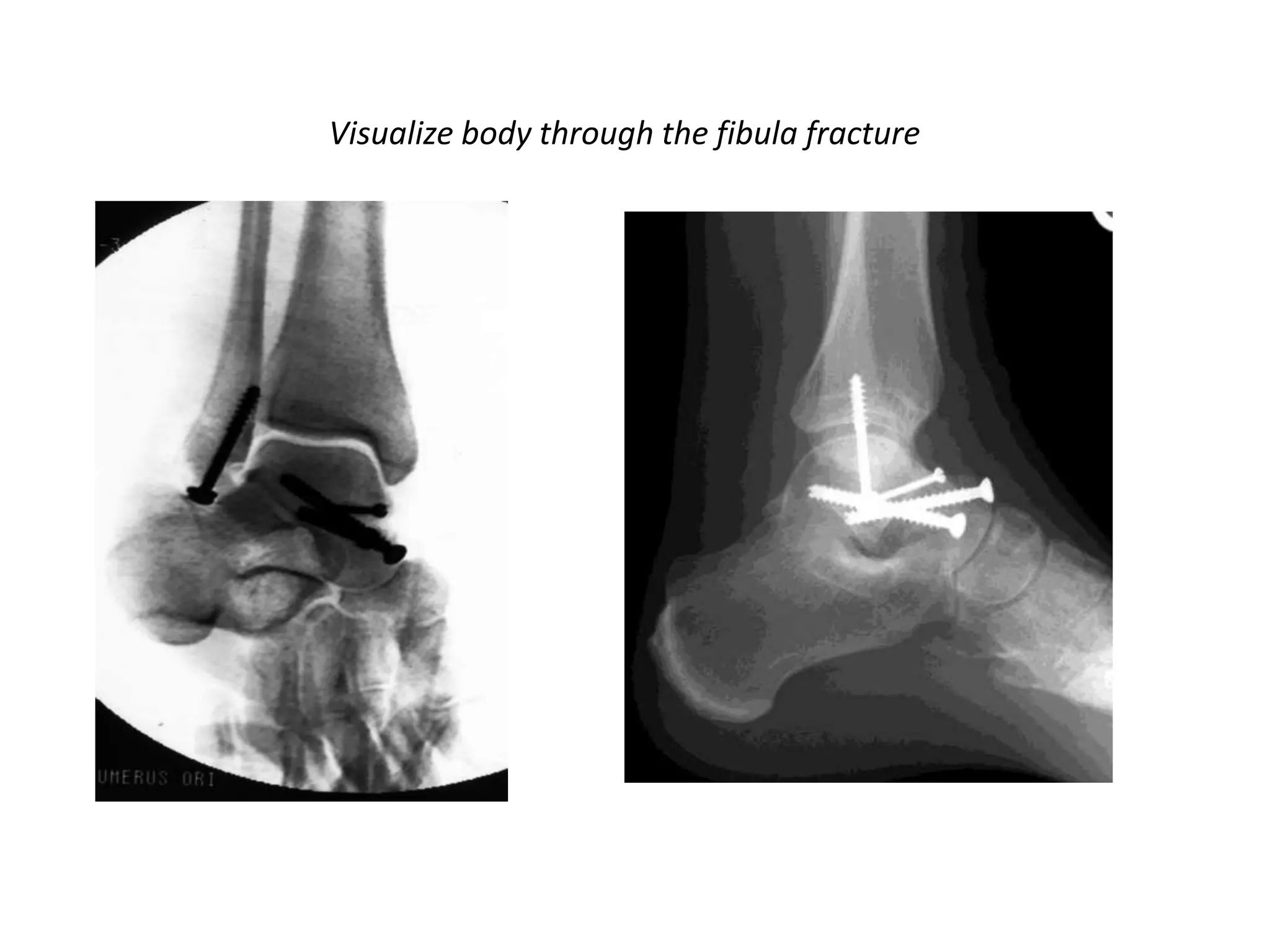
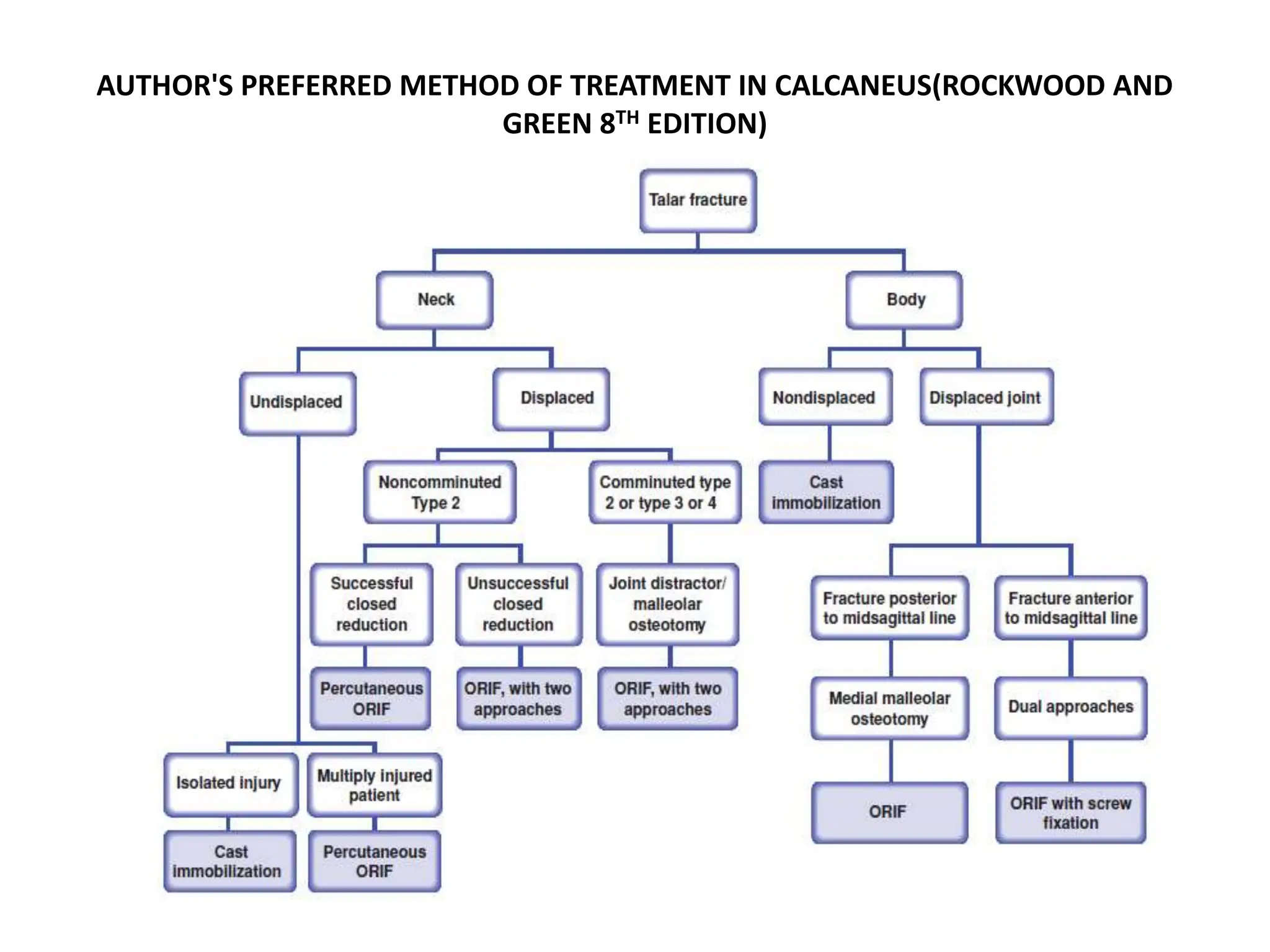
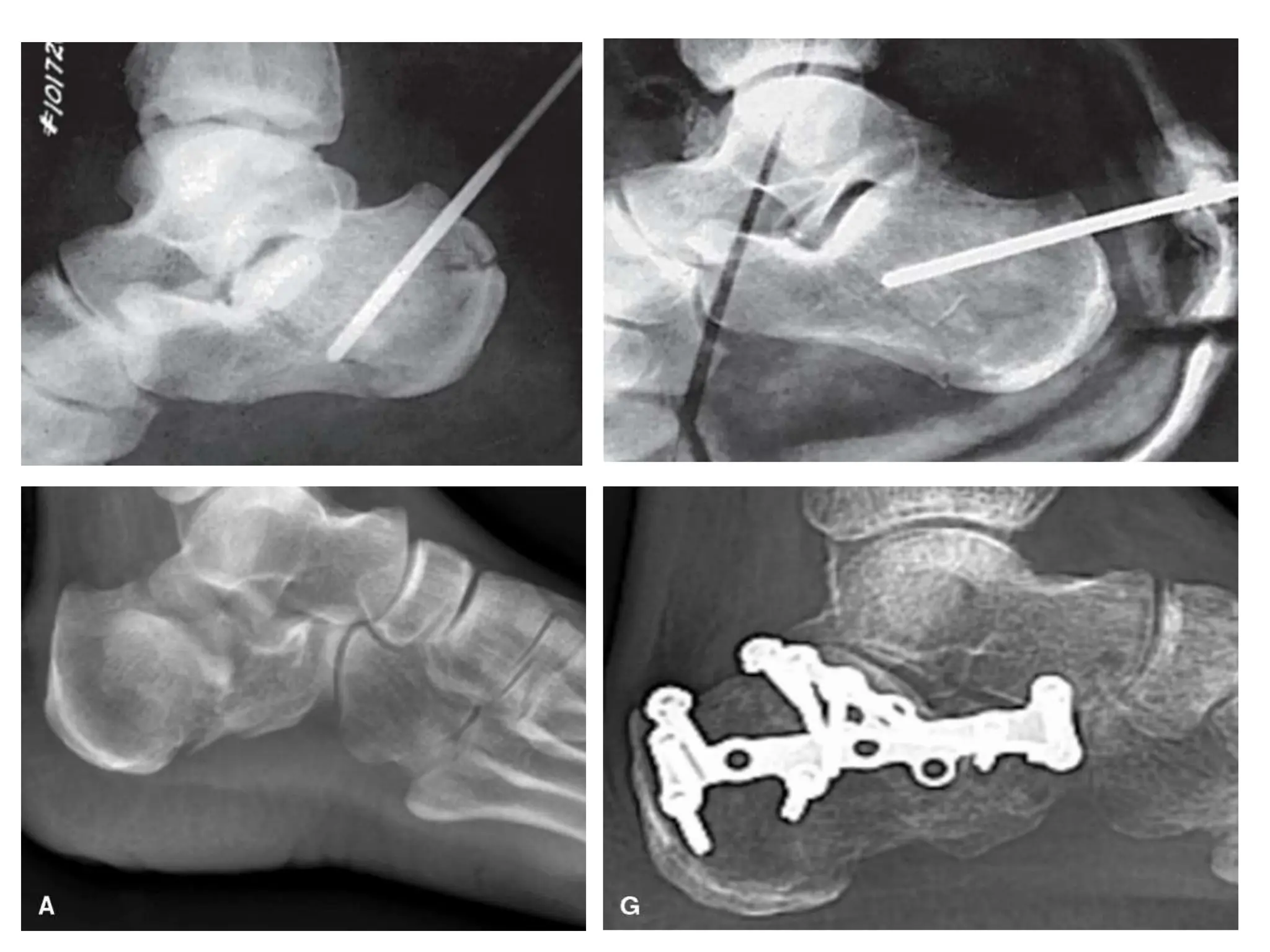
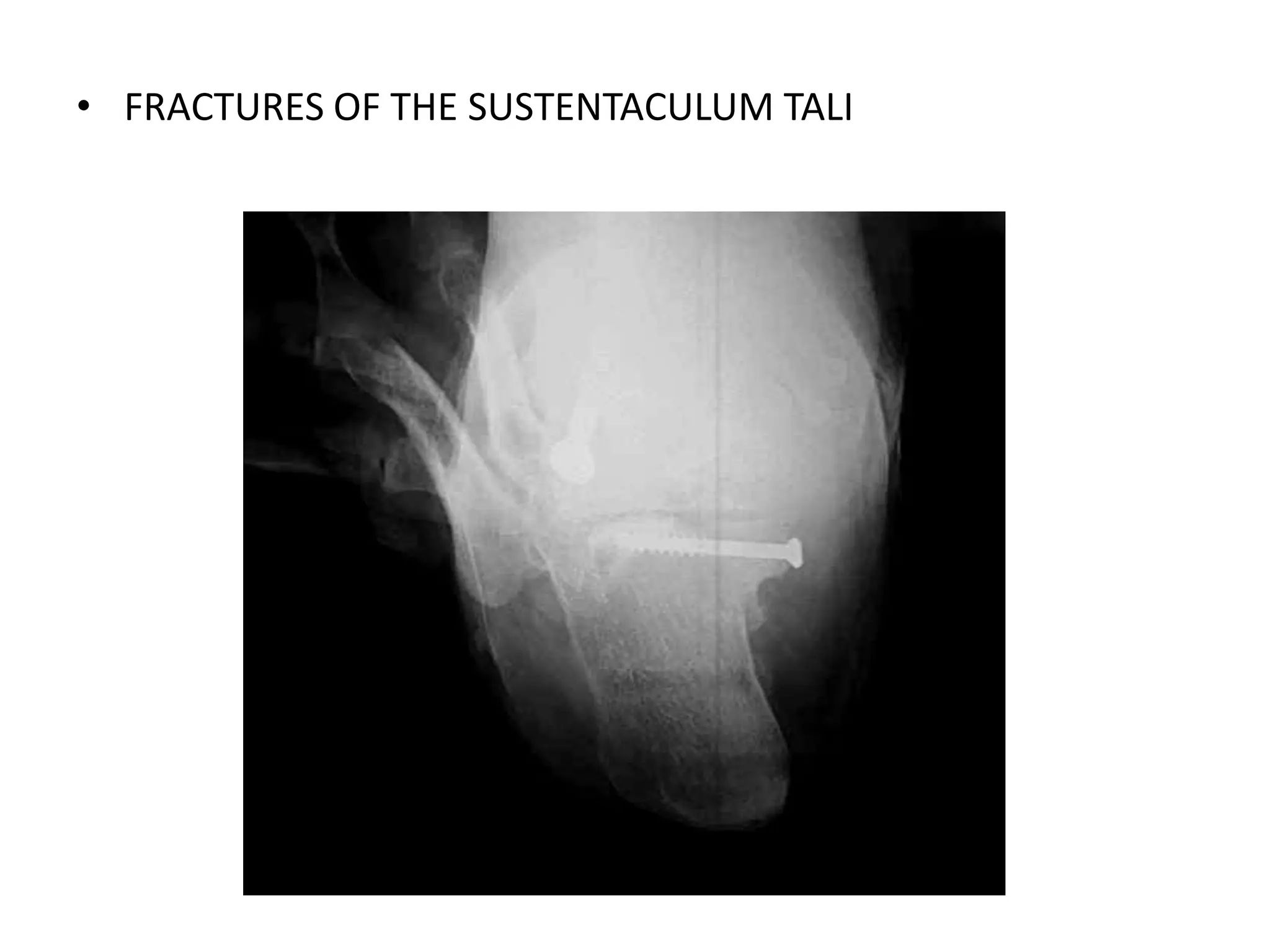
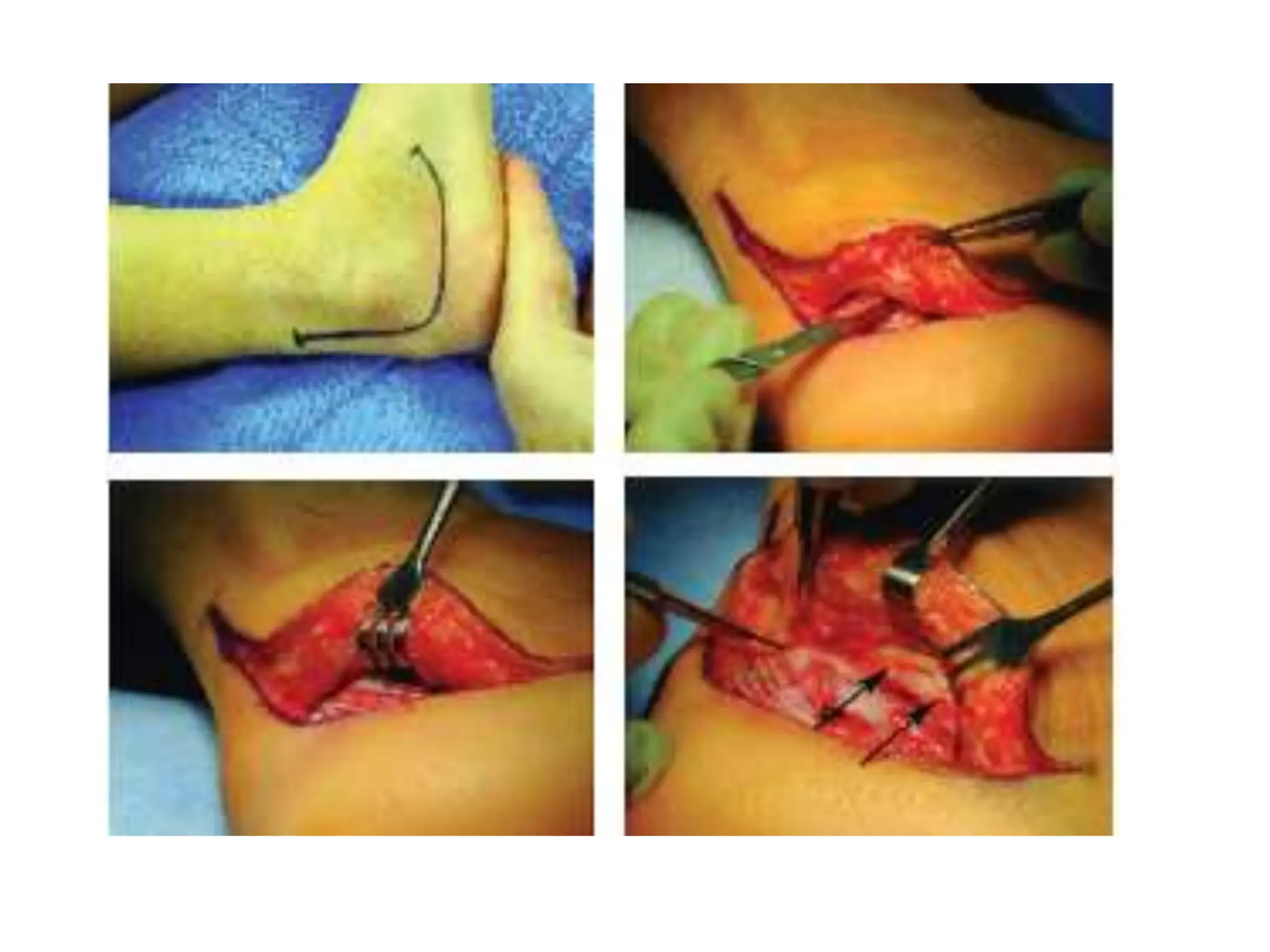
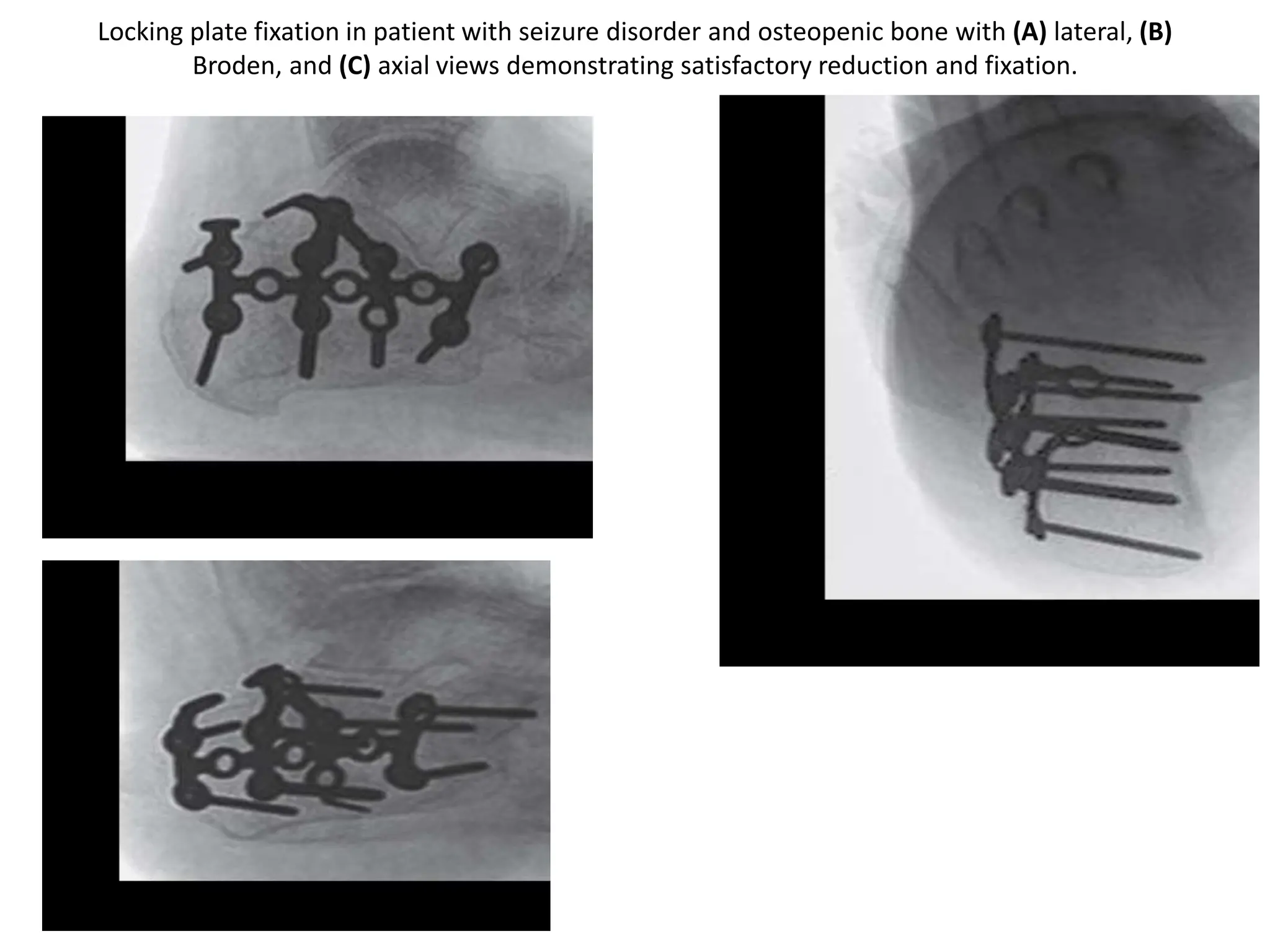
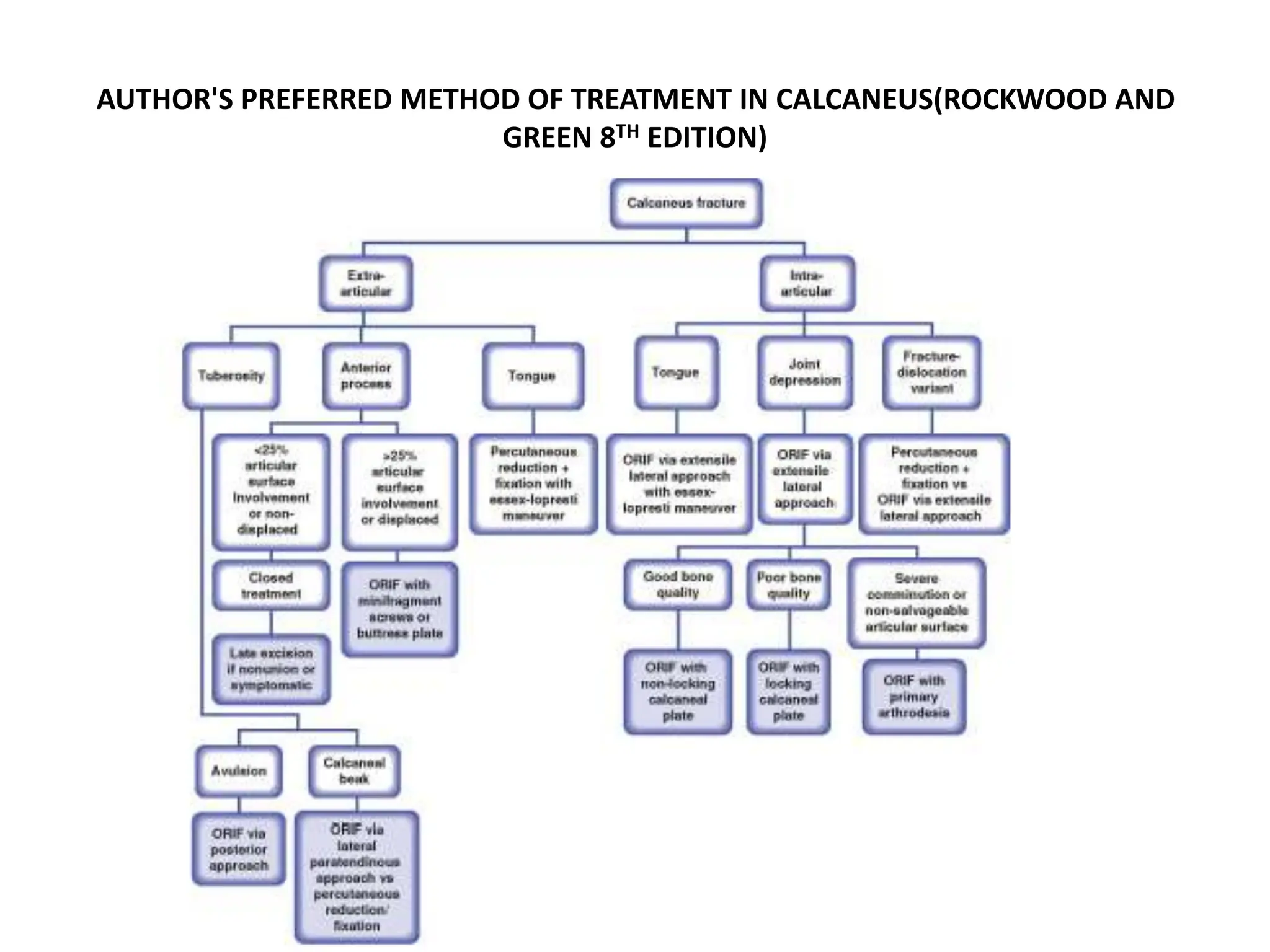
3) Treatment depends on fracture type but often involves open reduction and internal fixation to restore anatomy and allow early motion, in order to improve outcomes and reduce complications like malunion and avascular necrosis.