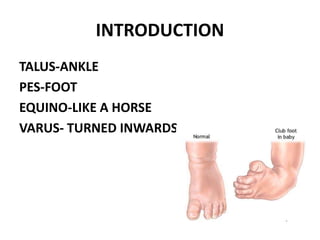
This document provides an overview of clubfoot (CTEV), including:
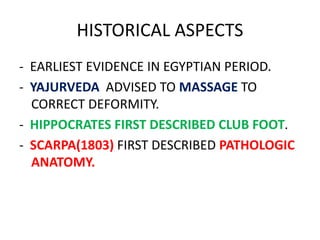
1. The historical aspects and key figures in the development of clubfoot treatment methods.
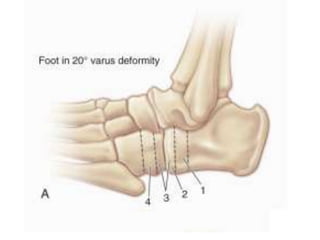
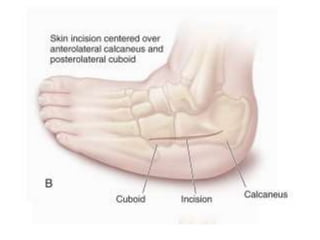
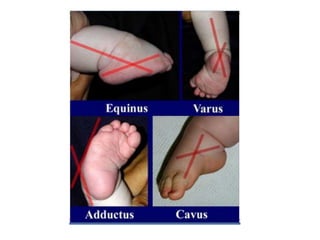
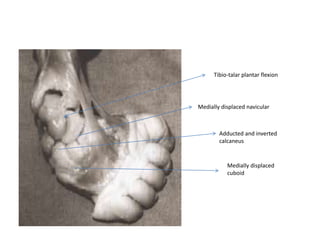
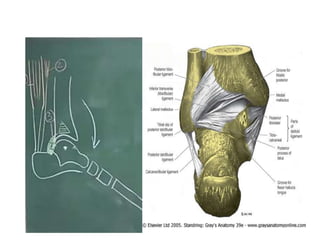
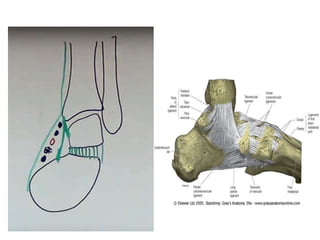
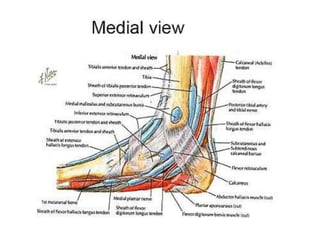
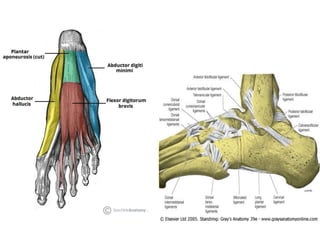
2. The anatomy and biomechanics involved in clubfoot deformity.
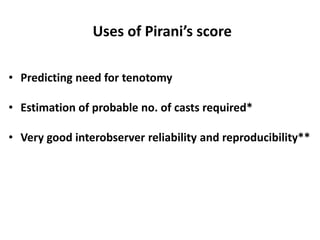
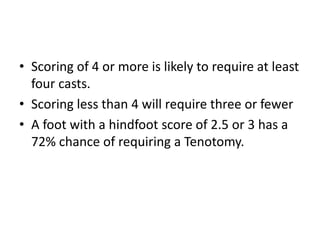
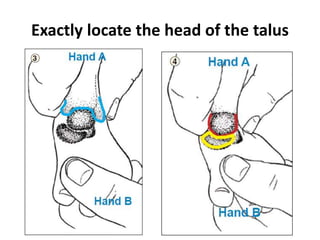
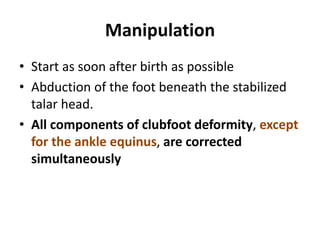
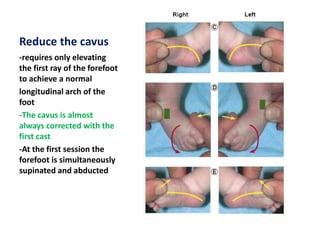
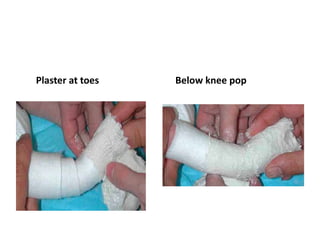
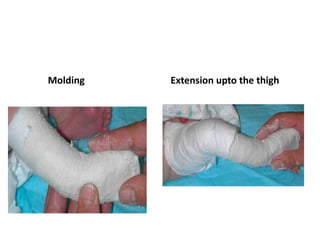
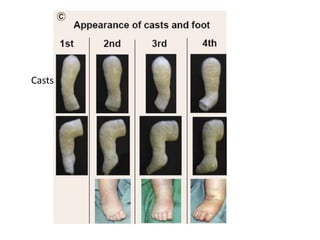
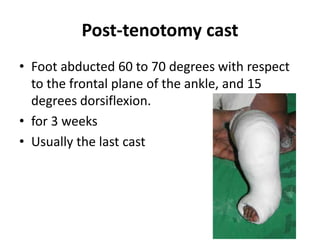
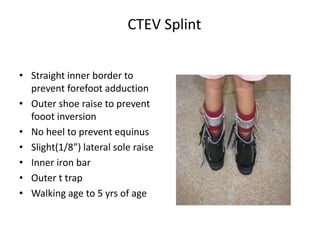
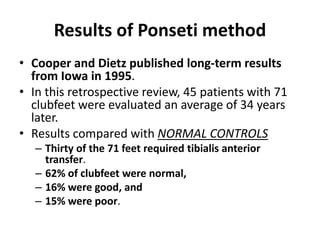
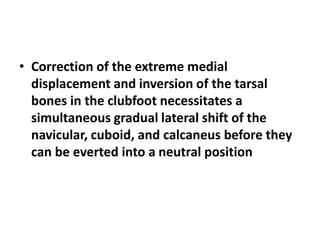
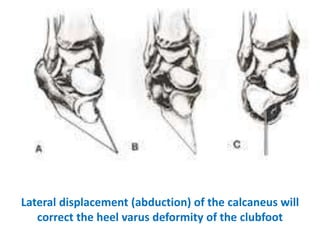
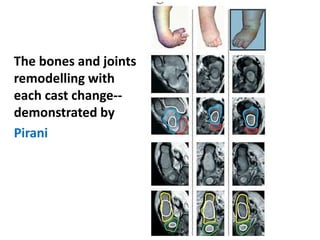
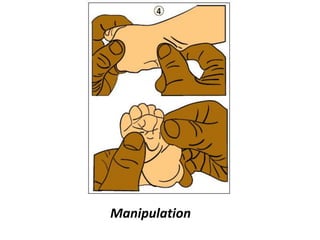
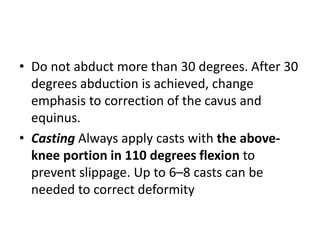
3. The Ponseti method of non-surgical clubfoot correction, which involves weekly manipulation, casting, and often a percutaneous Achilles tenotomy.
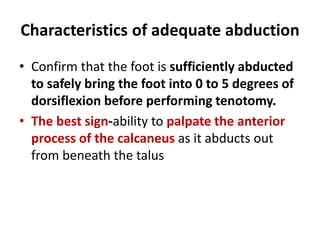
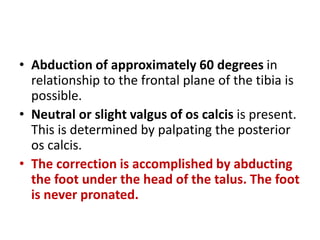
4. Important considerations for casting including proper manipulation technique and ensuring adequate foot abduction prior to tenotomy.
5. Potential complications of casting and the process of cast removal.









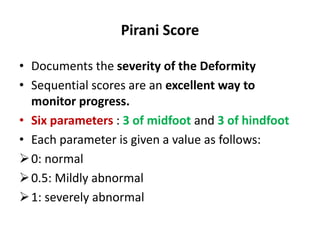
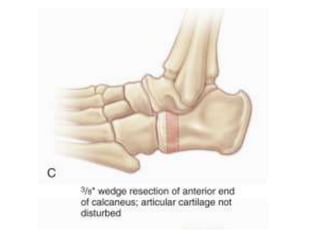
![Mid foot score
• Curved lateral border
[A]
• Medial crease [B]
• Talar head coverage [C]](https://image.slidesharecdn.com/ctev-171120174302/85/Ctev-63-320.jpg)
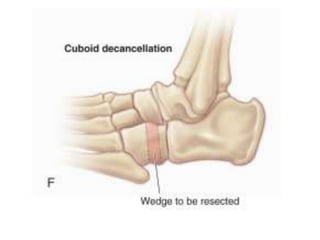
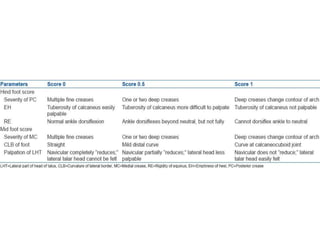
![Hind foot score
• Posterior crease [D]
• Rigid equinus [E]
• Empty heel [F]](https://image.slidesharecdn.com/ctev-171120174302/85/Ctev-64-320.jpg)