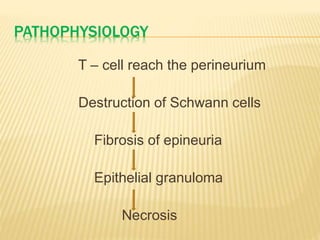
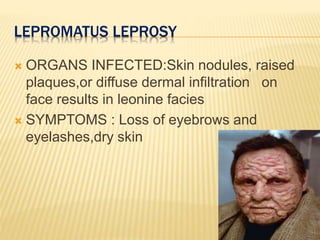
This document summarizes leprosy (Hansen's disease), caused by Mycobacterium leprae. It has an incubation period of 2-20 years and primarily affects the nerves, skin, eyes, and respiratory tract. Transmission occurs through direct contact with untreated patients or infected soil. Leprosy is classified into tuberculoid, lepromatous, borderline, and indeterminate forms based on symptoms and immune response. Tuberculoid leprosy causes localized skin lesions and nerve damage, while lepromatous leprosy results in widespread skin nodules and organ involvement. Diagnosis involves skin smears and biopsies examined microscopically. Treatment consists of multid