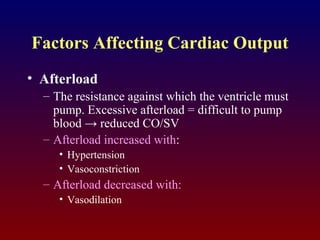
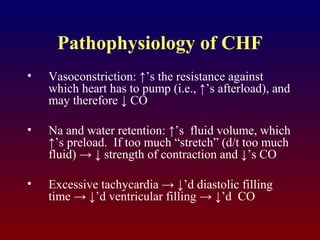
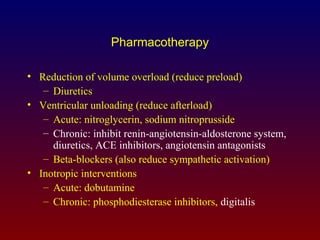
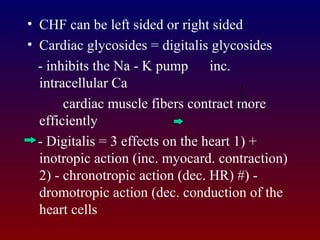
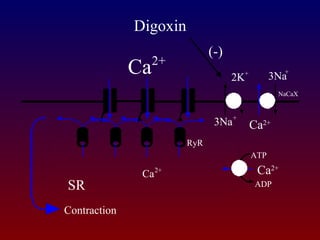
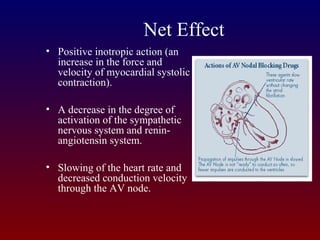
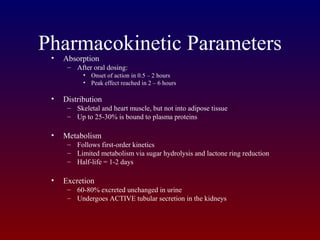
Congestive heart failure is a condition where the heart muscle is unable to pump enough blood to meet the body's needs. It can be caused by high blood pressure, heart attacks, heart rhythm problems, or valve disorders damaging the heart muscle over time. Digitalis is a cardiac glycoside drug that is often used to treat congestive heart failure by increasing the strength of heart muscle contractions and decreasing heart rate, which improves the heart's pumping ability. It works by inhibiting the sodium-potassium pump in heart cells. Common side effects include vision changes, nausea, diarrhea and bradycardia. Careful dosage adjustment is required based on individual factors and renal function.