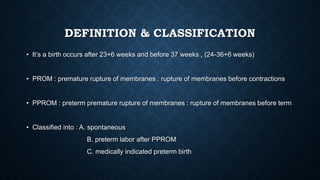
Preterm labor is defined as birth occurring between 23+6 and 36 weeks of gestation and is classified into spontaneous, after premature rupture of membranes (pprom), and medically indicated cases. Key risk factors include prior preterm labor, infections, multiple pregnancies, and uterine anomalies, with significant implications for neonatal outcomes. Management strategies involve tocolysis, corticosteroids for lung maturity, and interventions like cervical cerclage in high-risk women.