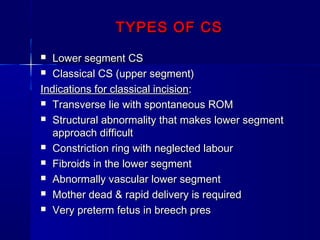
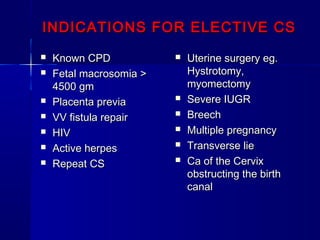
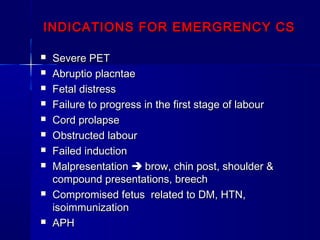
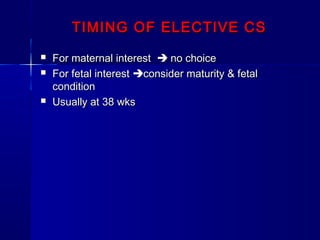
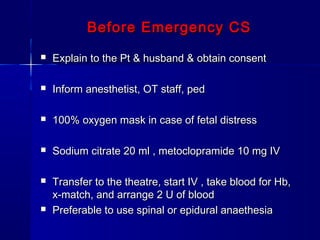
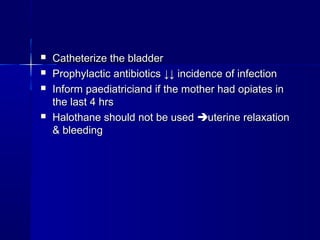
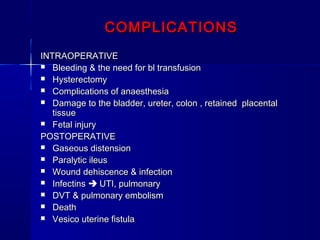
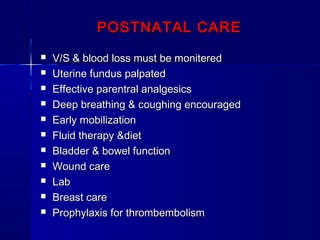
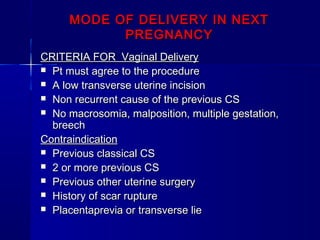
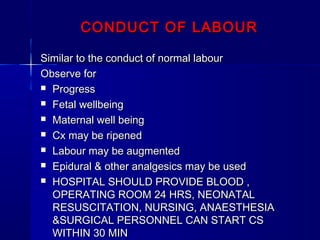
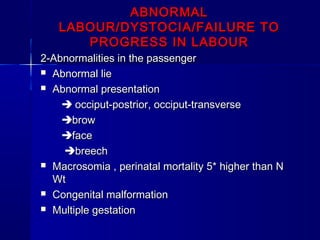
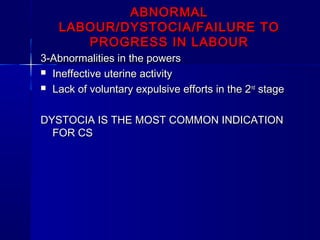
This document discusses cesarean section (CS), including types of CS, indications for elective and emergency CS, timing of elective CS, complications, postnatal care, and mode of delivery in subsequent pregnancies. It notes that lower segment CS and classical/upper segment CS are the main types. Indications include fetal malpresentation, failure to progress in labor, and prior uterine surgery. The timing of elective CS is usually 38 weeks. Complications can be intraoperative like bleeding or postoperative like infection. Strict postnatal care including monitoring is important. Vaginal delivery may be possible in subsequent pregnancies if certain criteria are met like a previous low transverse incision and no other risk factors.