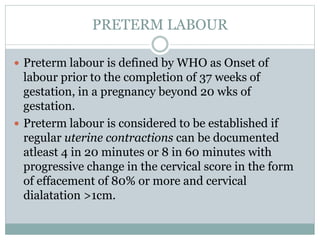
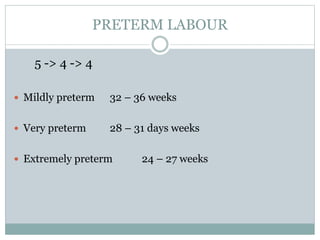
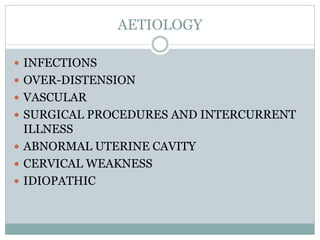
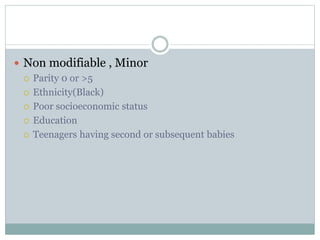
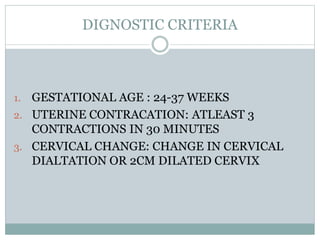
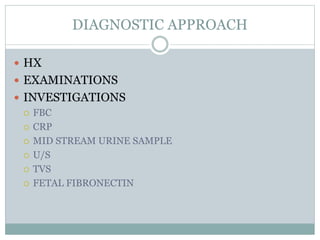
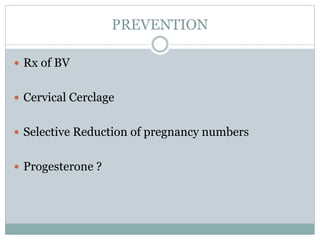
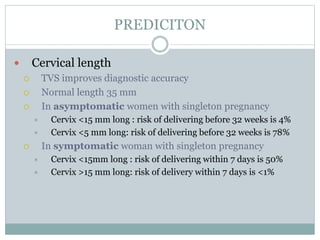
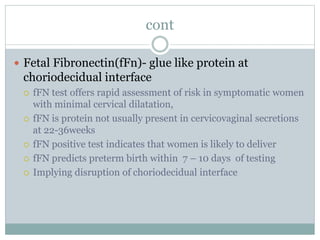
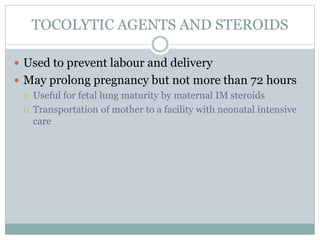
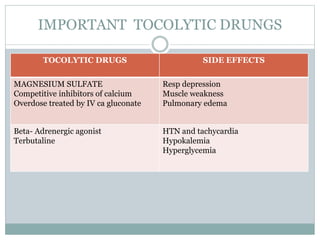
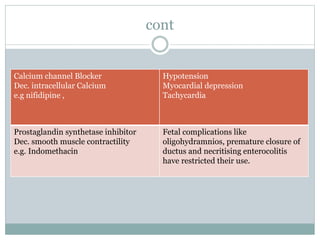
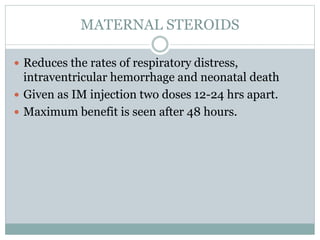
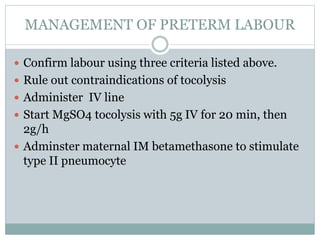
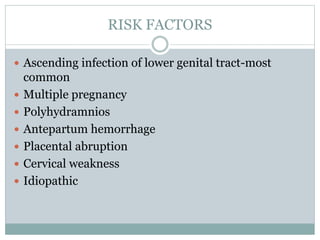
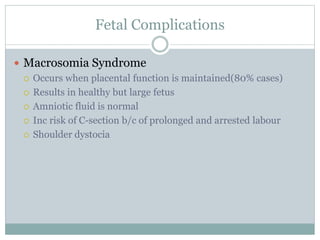
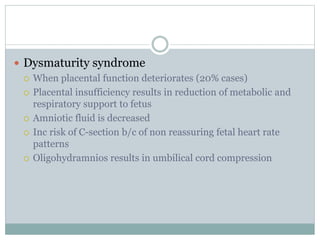
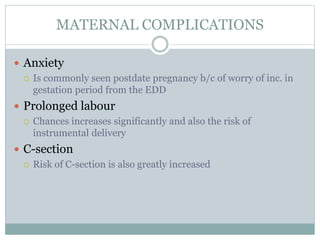
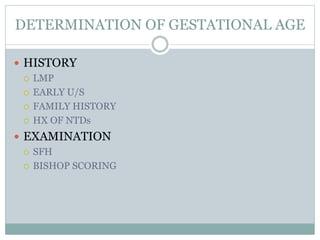
This document provides information on preterm and post-term labor. It defines preterm labor as onset of labor before 37 weeks of gestation and discusses the main risk factors, diagnosis, and management. Diagnosis requires documentation of regular contractions and cervical changes. Tocolytics and steroids are used to delay delivery. For post-term labor, it defines this as pregnancy exceeding 42 weeks and notes the risks include macrosomia, dystocia, and complications of prolonged labor. Conservative management or induction is recommended depending on cervical status and fetal well-being.