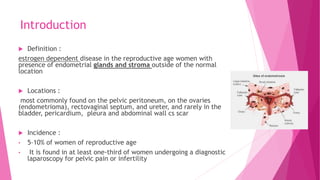
Endometriosis is an estrogen-dependent disease where endometrial tissue grows outside the uterus, most commonly on the pelvic peritoneum and ovaries. It affects 5-10% of women and is a common cause of pelvic pain and infertility. While the exact cause is unknown, theories include retrograde menstruation through the fallopian tubes and genetic or immunological factors. Diagnosis involves laparoscopy to visualize lesions, and ultrasound or MRI may also help. Treatment depends on symptoms but may include pain medications, hormonal therapy, or surgery to remove growths or the ovaries/uterus. Surgical treatment can help fertility in mild-moderate cases.