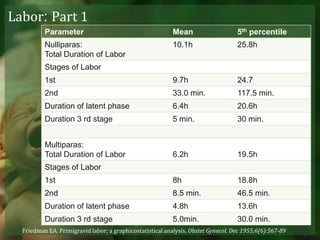
Labor is a complex process involving biochemical and hormonal changes that lead to coordinated uterine contractions, cervical dilation, and ultimately delivery. Accurate dating of pregnancy is essential for distinguishing between normal and abnormal labor conditions, with various phases of labor defined from onset to delivery of the neonate and placenta. Changes in maternal and fetal characteristics have influenced contemporary labor patterns, necessitating careful assessment to manage potential dysfunctional labor.
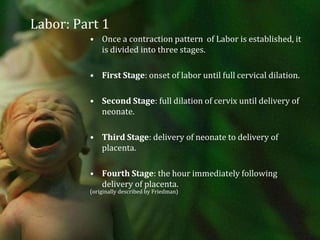
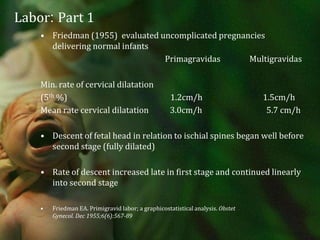
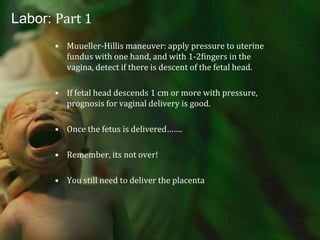
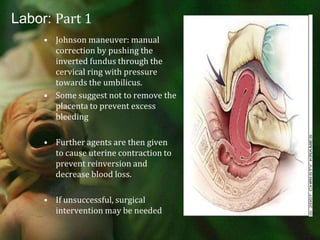
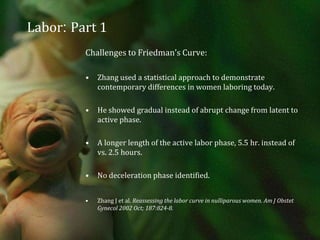
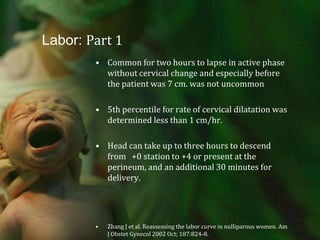
![Labor: Part 1Recent challenges to Friedman’s data on patient’s labor patterns reflects changes over the past 50 years in the patients we see and how we practice. More aggressive medical management, higher induction rates, use of oxytocin, regional anesthesia and continuous fetal monitoring. Maternal characteristics have also changed, with greater body mass index [BMI] and an increase in fetal size.](https://image.slidesharecdn.com/laborpartone-110729003437-phpapp02/85/Labor-part-one-32-320.jpg)
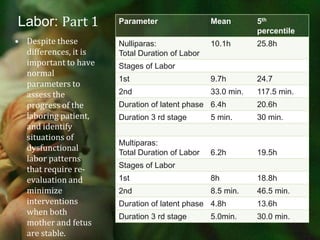

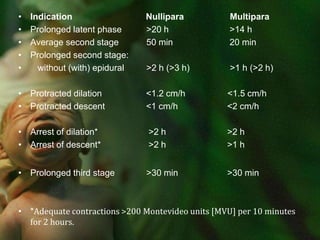
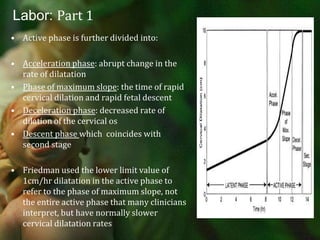
![Indication Nullipara Multipara Prolonged latent phase >20 h >14 h Average second stage 50 min 20 min Prolonged second stage: without (with) epidural >2 h (>3 h) >1 h (>2 h) Protracted dilation <1.2 cm/h <1.5 cm/h Protracted descent <1 cm/h <2 cm/h Arrest of dilation* >2 h >2 h Arrest of descent* >2 h >1 hProlonged third stage >30 min >30 min *Adequate contractions >200 Montevideo units [MVU] per 10 minutes for 2 hours.](https://image.slidesharecdn.com/laborpartone-110729003437-phpapp02/85/Labor-part-one-46-320.jpg)