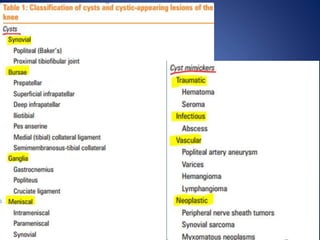
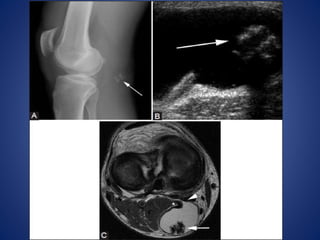
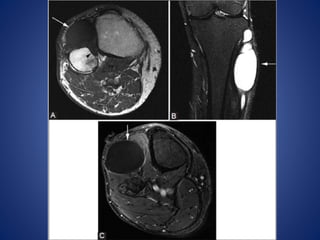
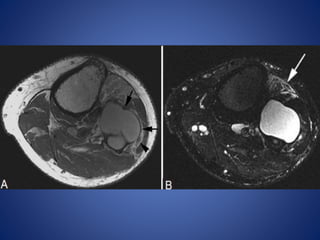
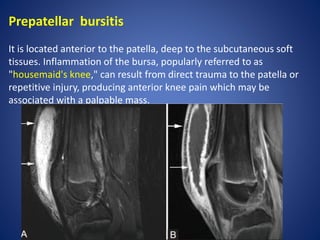
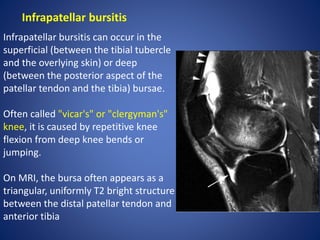
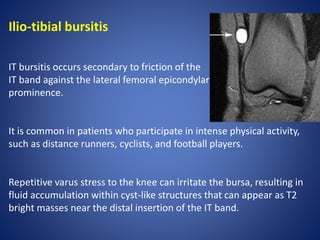
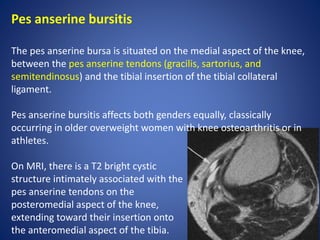
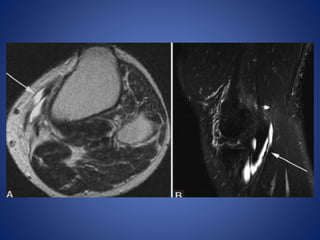
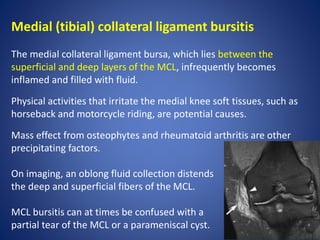
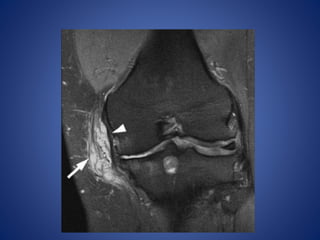
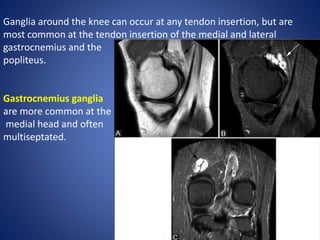
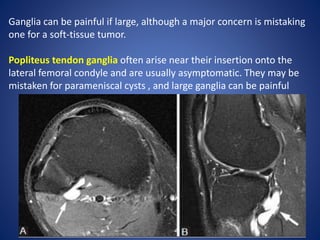
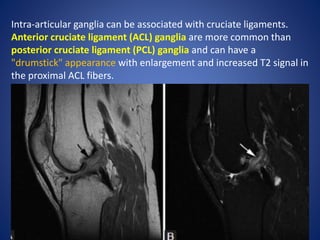
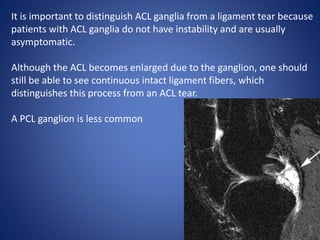
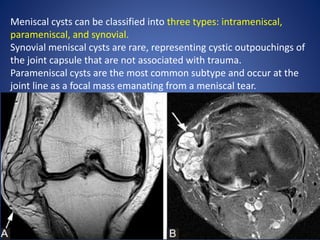
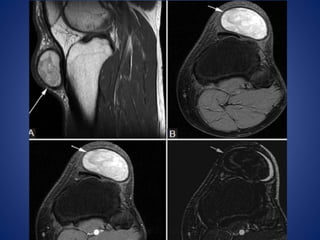
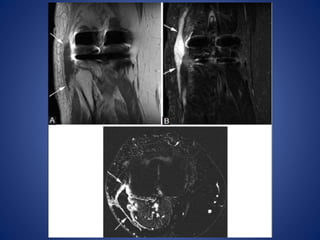
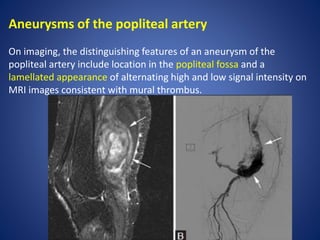
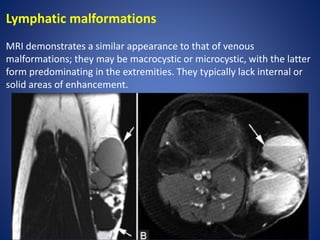
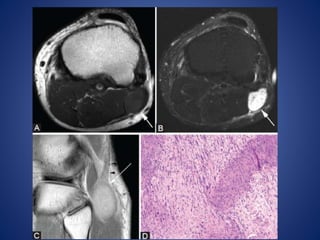
This document summarizes various cysts and cyst-like lesions that can occur in the knee. It describes popliteal (Baker's) cysts as the most common knee cyst, which forms due to a connection between the posterior joint capsule and gastrocnemius-semimembranosus bursa. It also discusses proximal tibiofibular joint cysts, bursae such as prepatellar and infrapatellar bursitis, ganglia, meniscal cysts, and cyst mimickers including hematomas, seromas, vascular lesions, and neoplasms. Key distinguishing imaging features of different lesions are provided.