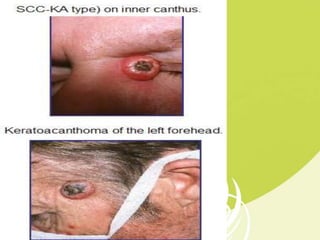
This document provides information on keratoacanthoma, a benign skin tumor that originates in hair follicles. It discusses the epidemiology, risk factors, clinical features, signs and symptoms, histopathology, differential diagnosis, investigations, management and treatment options. Keratoacanthoma typically presents as a rapidly growing nodule on sun-exposed skin and can resolve spontaneously within months, though complete excision is the treatment of choice.