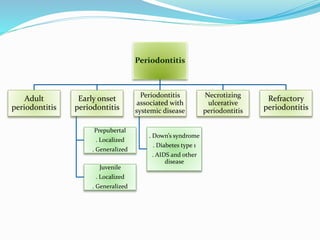
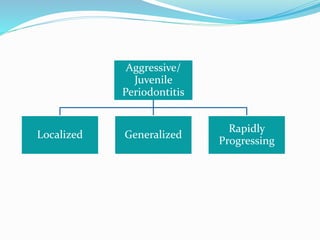
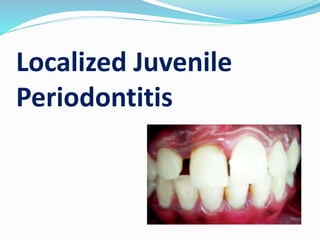
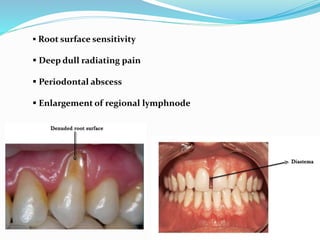
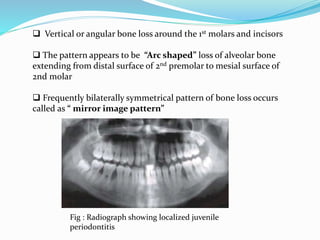
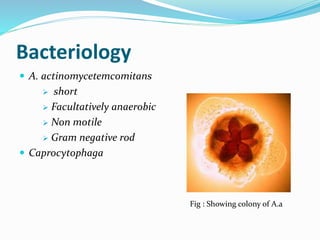
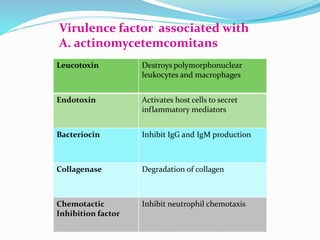
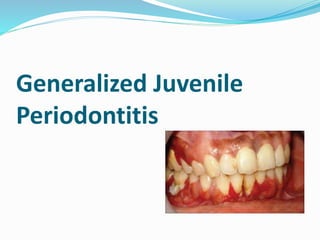
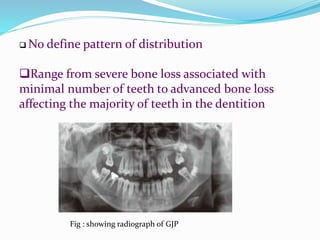
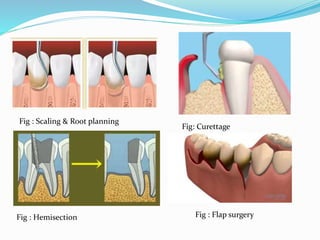
Juvenile periodontitis is a type of periodontitis that occurs in otherwise healthy individuals under 30 years old. It is characterized by rapid attachment and bone loss. There are two types: localized juvenile periodontitis, which is destructive to the first molars and incisors, and generalized juvenile periodontitis, which affects at least three teeth besides the first molars and incisors. Both types are caused by specific microorganisms like Actinobacillus actinomycetemcomitans and have features like deep pockets despite minimal plaque. Treatment involves scaling, root planing, antibiotics, and sometimes surgery.