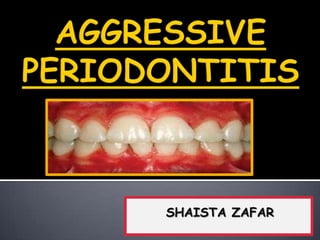
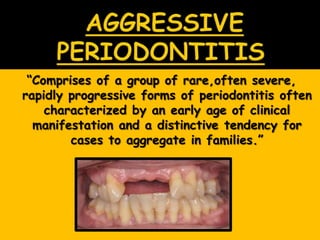
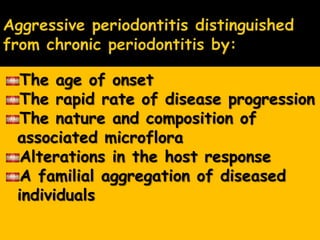
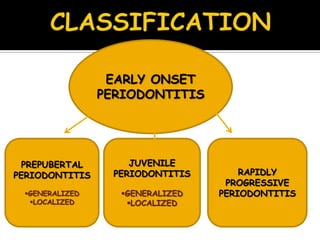
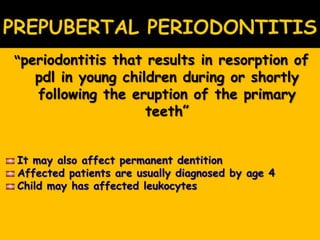
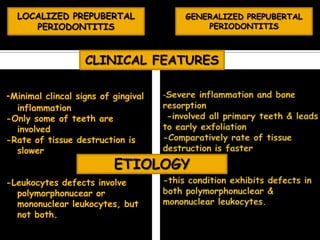
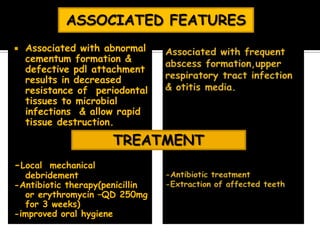
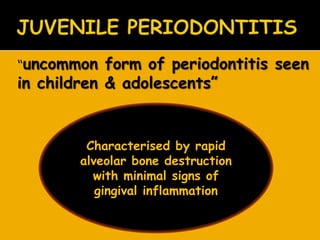
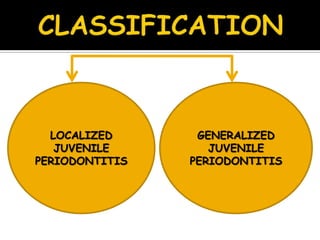
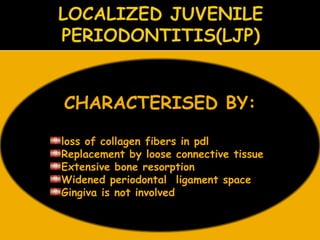
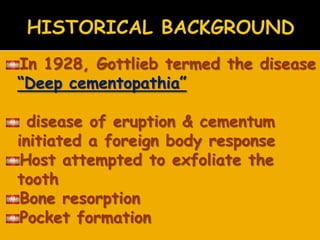
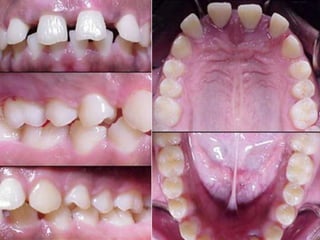
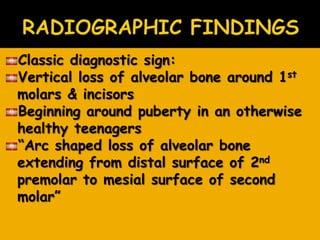
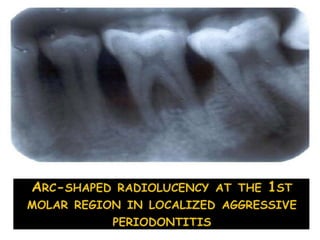
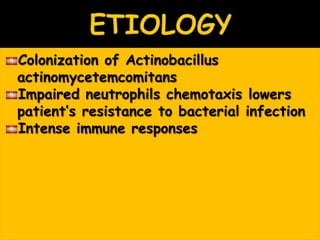
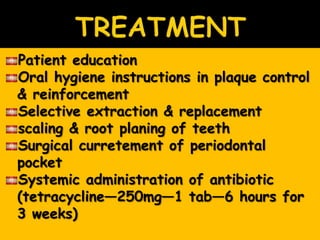
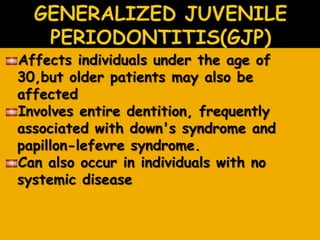
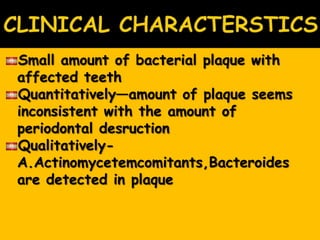
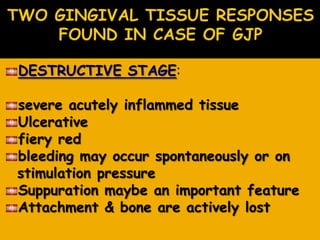
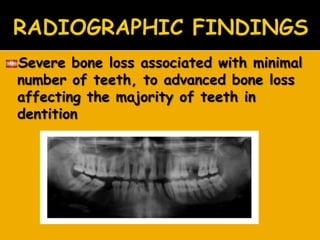
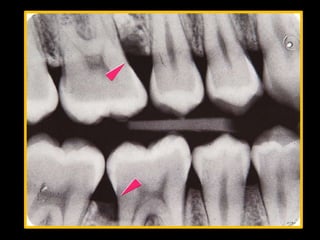
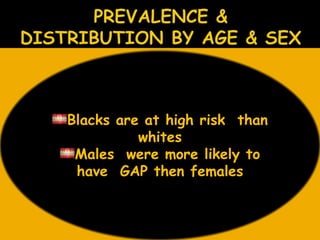
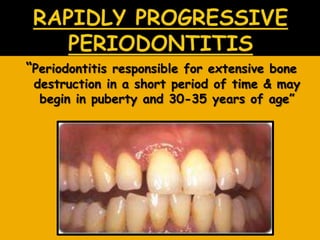
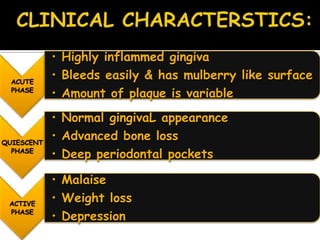
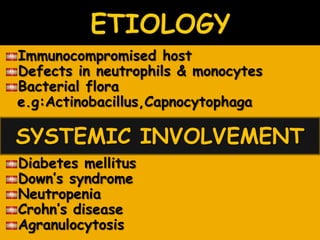
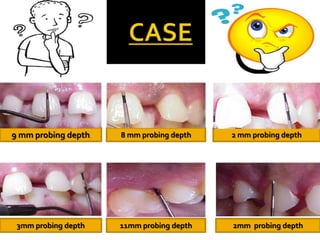
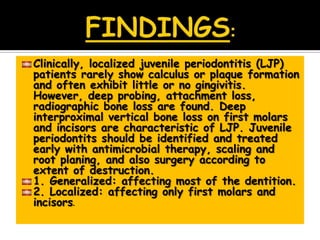
This document discusses early onset periodontitis, which comprises rare, severe, and rapidly progressive forms of periodontitis characterized by an early age of onset and familial aggregation. It describes several types including prepubertal, juvenile, and rapidly progressive periodontitis. Localized juvenile periodontitis is highlighted, which clinically presents with deep probing depths, attachment loss, and radiographic bone loss localized to first molars and incisors in otherwise healthy teenagers, despite minimal plaque and gingivitis. Treatment involves nonsurgical and surgical approaches along with antibiotic therapy.