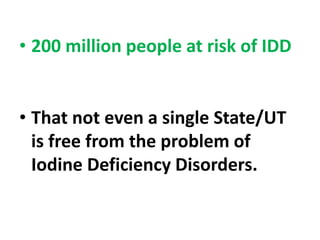
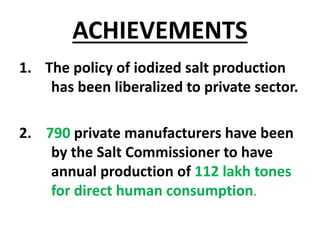
The document discusses India's National Iodine Deficiency Disorder Control Programme. It notes that iodine deficiency can cause goiter and other health issues. The programme aims to provide iodized salt to at-risk regions, educate the public, and monitor iodine levels. Key objectives include assessing iodine deficiency, supplying iodized salt, education, and monitoring impacts. The programme was later expanded to promote universal iodized salt consumption and strengthen monitoring.