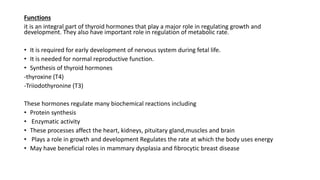
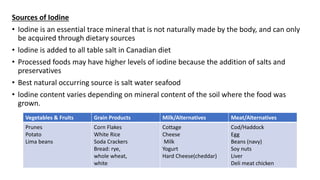
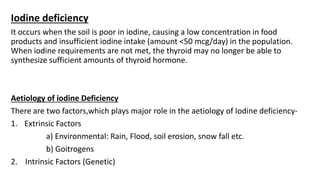
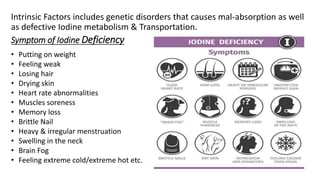
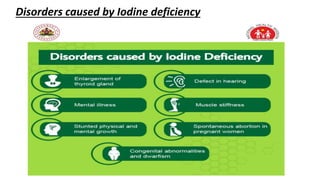
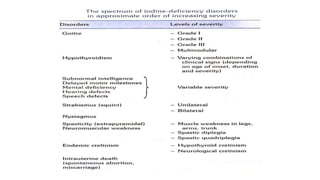
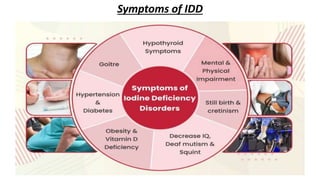
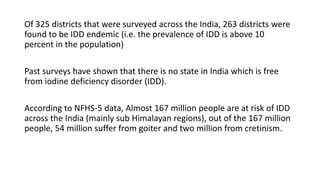
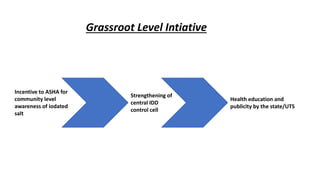
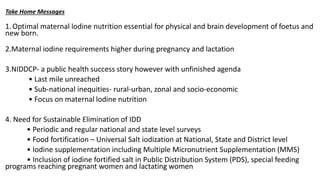
Iodine is an essential trace element needed to synthesize thyroid hormones. Nearly 80% of iodine in the body is stored in the thyroid gland. Iodine is absorbed from dietary sources like iodized salt and is transported to the thyroid via sodium/iodide symporters, where it is used to produce thyroid hormones that regulate growth, metabolism and brain development. Iodine deficiency can cause a spectrum of disorders and remains a public health issue in many parts of the world including India, where programs aim to ensure adequate iodine intake through universal salt iodization and health education.