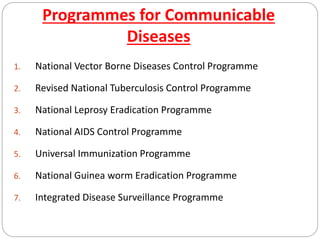
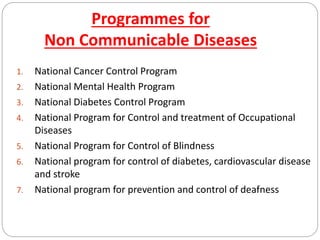
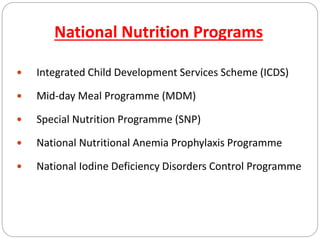
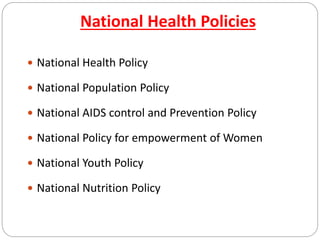
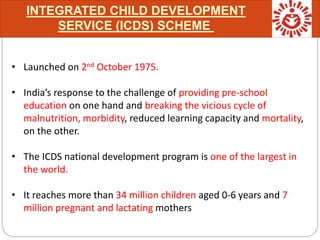
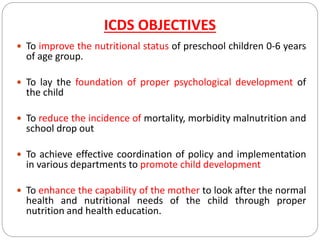
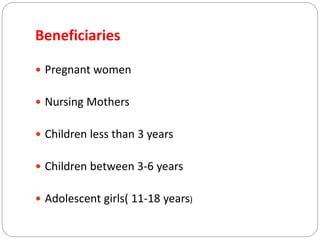
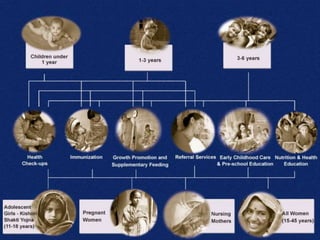
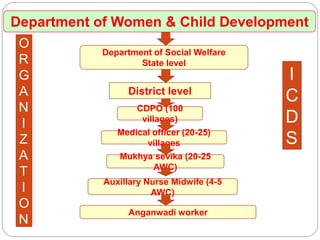
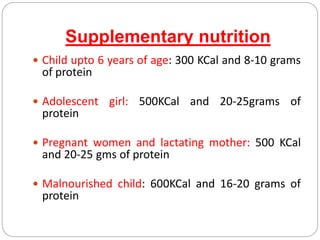
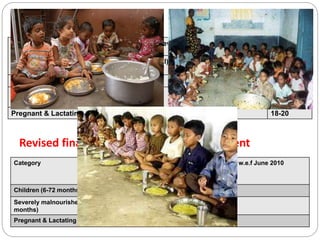
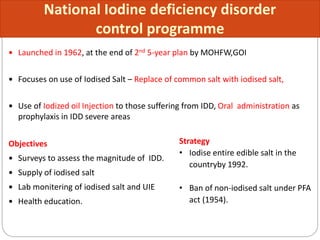
This document outlines several national health programmes and policies in India, including programmes for communicable diseases, non-communicable diseases, and nutrition. It provides details on major nutrition programmes like the Integrated Child Development Services (ICDS) scheme, mid-day meal programme, and national programmes addressing issues like anemia, iodine deficiency, and vitamin A deficiency. The ICDS is described as India's largest child development programme, reaching over 34 million children and 7 million mothers. It aims to improve child nutrition and reduce mortality and morbidity through Anganwadi centers that provide food, immunizations, health checkups, and preschool education.