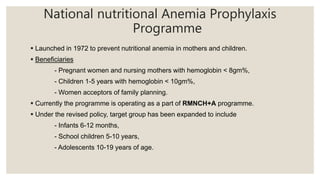
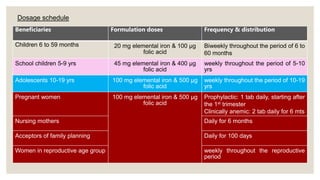
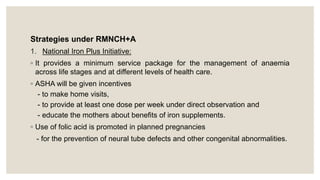
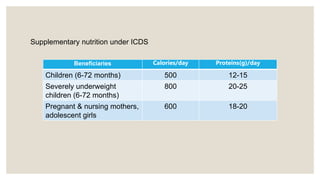
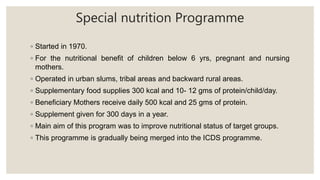
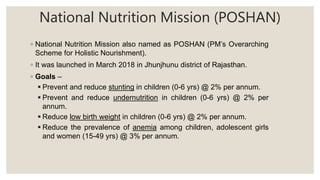
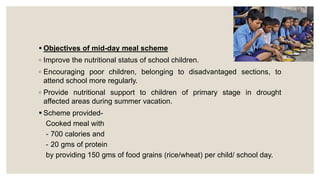
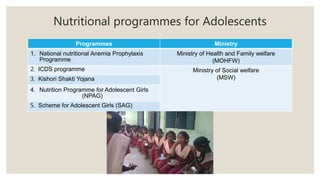
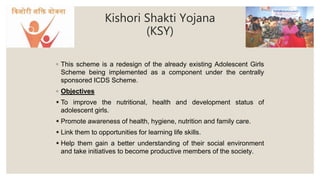
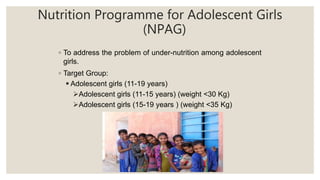
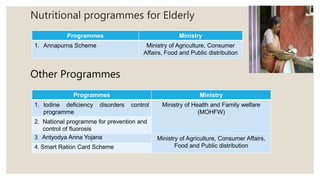
This document provides an overview of various community nutritional programmes in India. It discusses programmes targeted at pregnant and lactating mothers, children, adolescents, and elderly individuals. The key programmes described include the Integrated Child Development Services (ICDS) programme, National Nutritional Anemia Prophylaxis Programme, Mid-Day Meal programme, Vitamin A prophylaxis programme, and programmes under the Poshan Abhiyaan (National Nutrition Mission). The document provides details on the objectives, target groups, and services provided by these various nutritional programmes in India.