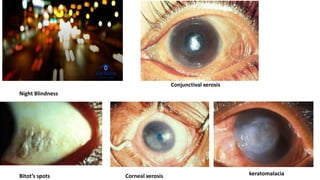
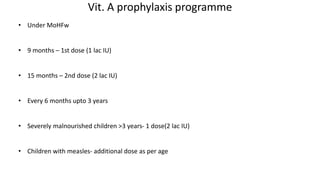
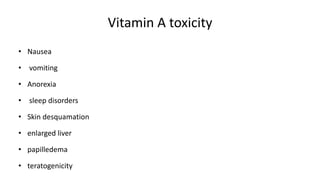
This document discusses vitamin A, including its functions, sources, deficiency, treatment, prevention, and toxicity. It notes vitamin A is important for vision, epithelial and glandular tissue, skeletal growth, immunity, and preventing epithelial cancers. Sources include animal liver, eggs, and fortified foods. Deficiency can cause night blindness, spots on the eye, skin issues, growth problems, and increased infection risk. Treatment is high dose vitamin A supplements. Prevention involves a diet with vitamin A foods and reducing illness risk factors. India has a vitamin A prophylaxis program providing supplements to children. Toxicity from too much vitamin A can cause nausea, vomiting, skin issues and liver problems.