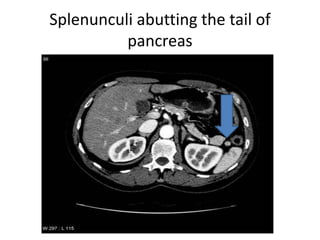
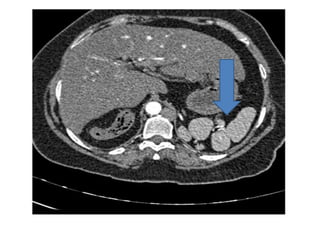
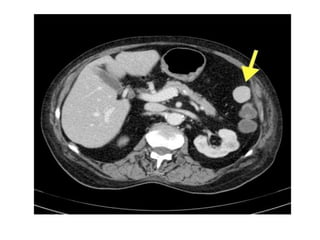
The spleen is located in the left upper quadrant of the abdomen. It filters blood and fights infections. The spleen develops from embryonic tissue and is supplied by the splenic artery and drained by the splenic vein. It can vary in size and shape. Accessory spleens are common. Injuries from trauma are most often seen in the spleen. Conditions like infections, cancers, blood disorders can cause abnormalities. Imaging with ultrasound, CT scan, MRI and nuclear medicine scans are used to evaluate the spleen.