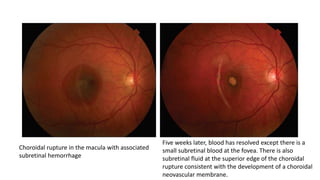
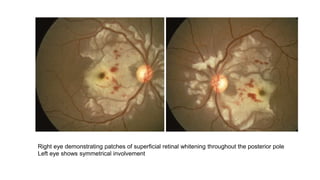
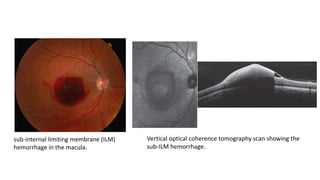
Traumatic chorioretinal pathologies can result from both penetrating and non-penetrating ocular injuries. Males under 40 are most commonly affected. Closed globe injuries may cause commotio retinae, while open globe injuries risk choroidal rupture. Indirect injuries like Valsalva retinopathy or Terson syndrome can also cause intraocular bleeding. Traumatic macular holes and retinal detachments require surgical repair like vitrectomy. Overall ocular trauma remains a major cause of blindness worldwide.