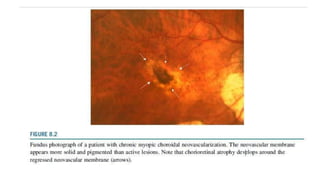
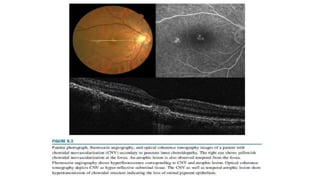
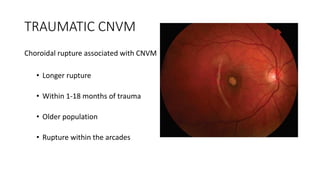
This document discusses non-AMD causes of choroidal neovascularization (CNV). It describes how CNV can be caused by degenerative diseases like high myopia, inflammatory diseases like uveitis, trauma, tumors, and idiopathically. For each cause, it discusses the pathogenesis, diagnosis using techniques like fluorescein angiography and OCT, and treatment options including anti-VEGF agents and laser photocoagulation. Radiance and MyrrOR trials showed effectiveness of anti-VEGF for treating myopic CNV specifically. CNV has various presentations and complications depending on the underlying cause.