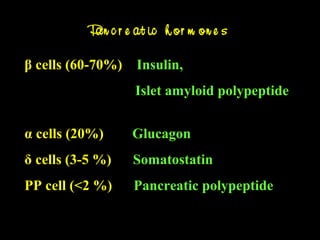
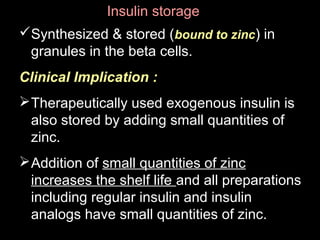
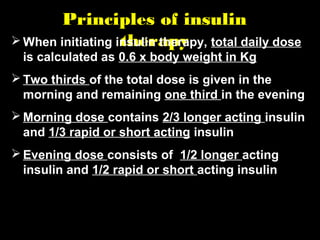
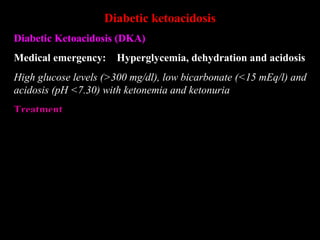
Treatment of Type 1 Diabetes mellitus involves lifelong insulin administration. Insulin is produced in the pancreas and regulates blood glucose levels. Type 1 diabetes results from autoimmune destruction of insulin-producing pancreatic beta cells leading to complete insulin deficiency. Various insulin preparations have been developed with differing durations of action to mimic normal insulin secretion. Treatment involves calculating total daily insulin dose and dividing into short and long-acting insulins administered multiple times daily. Adverse effects and methods to overcome insulin resistance are also discussed.