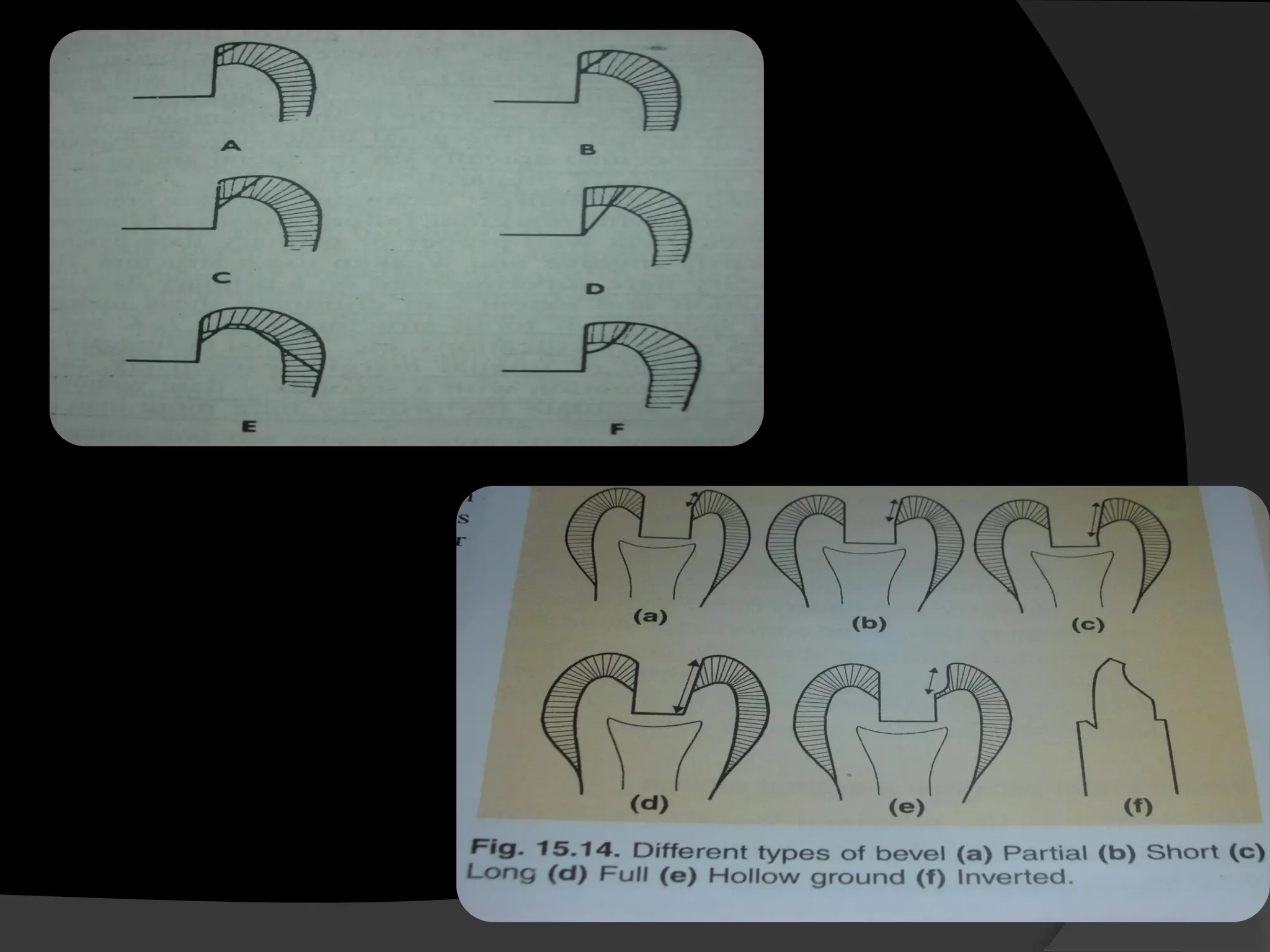
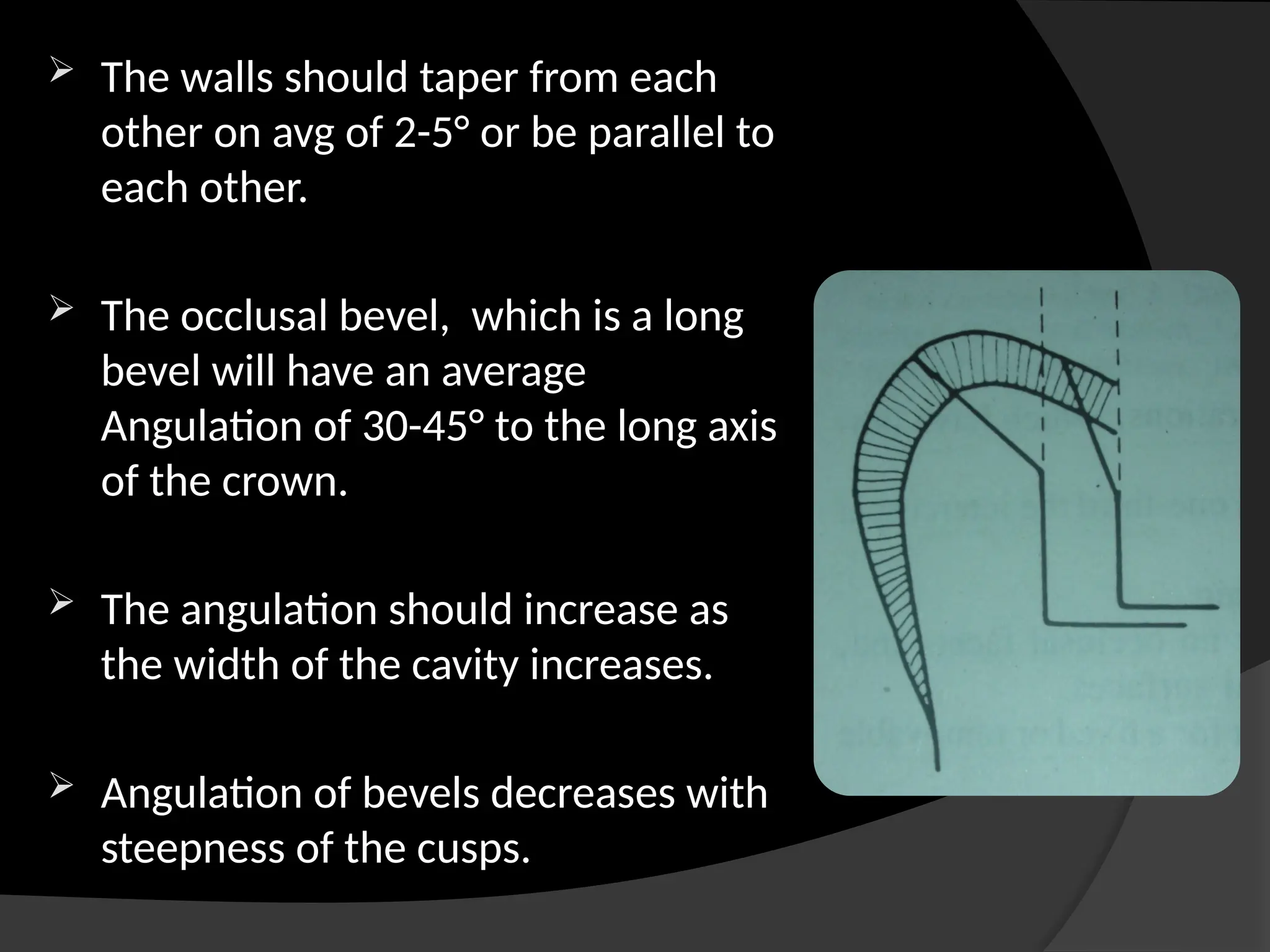
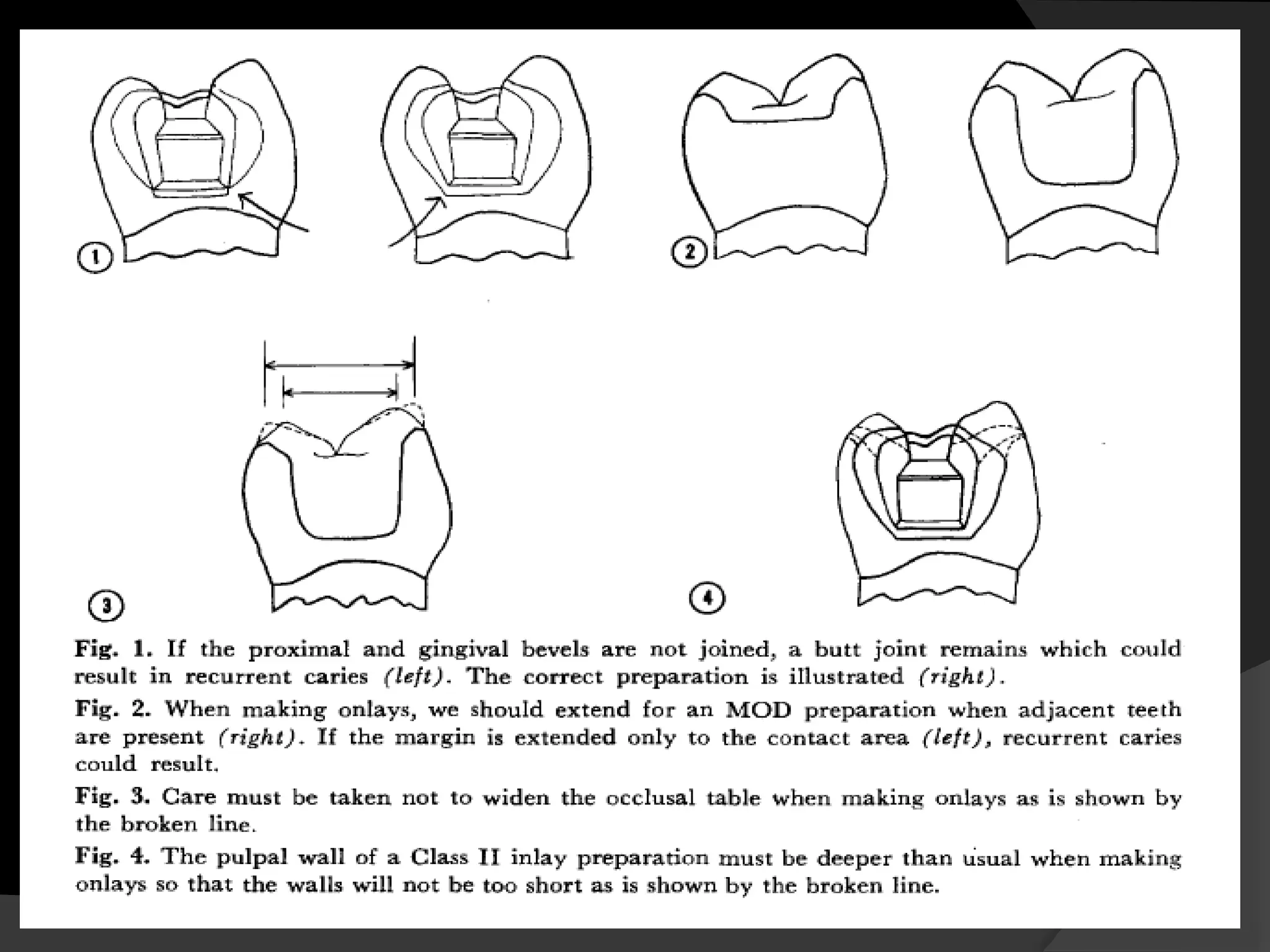
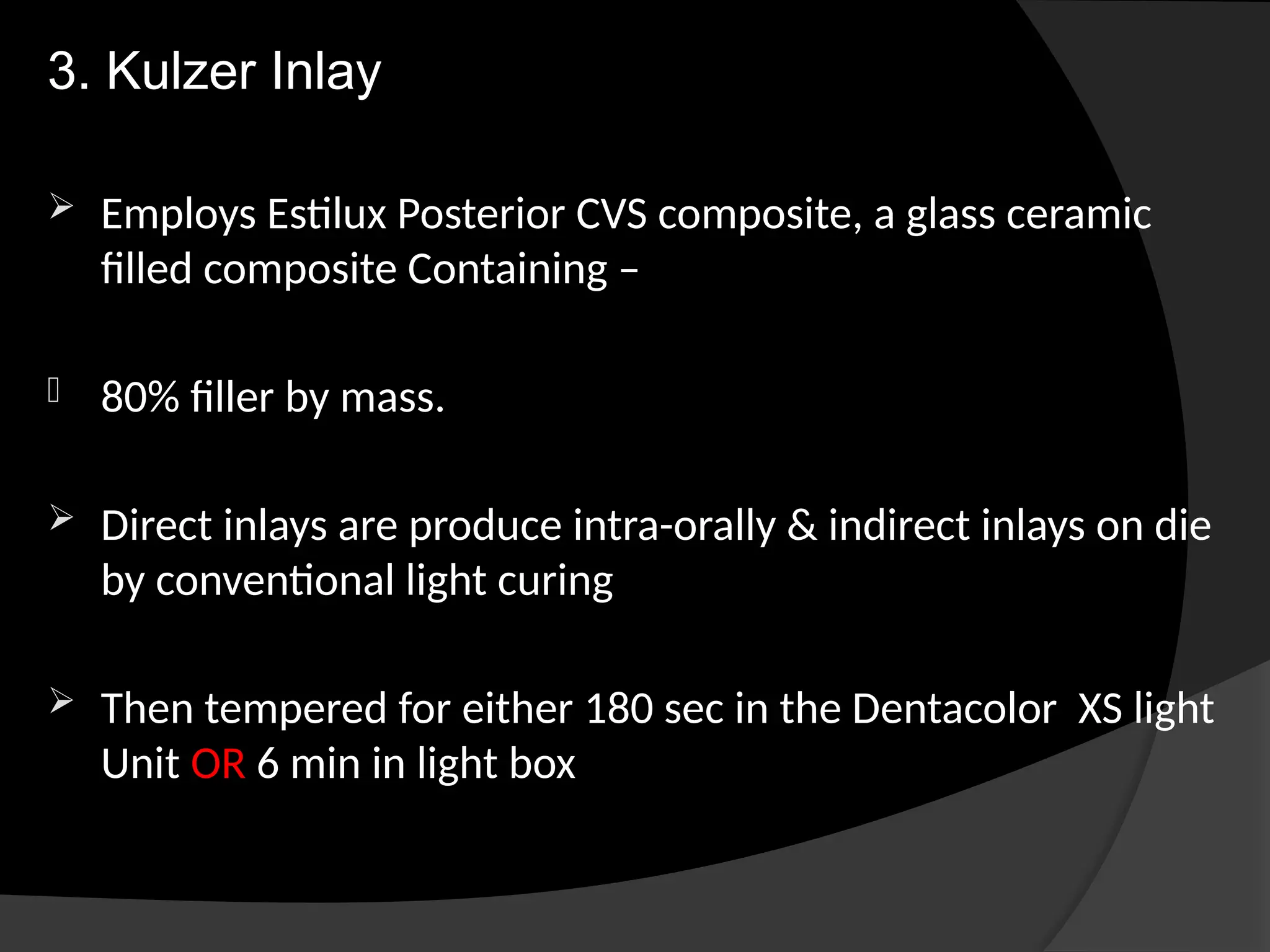
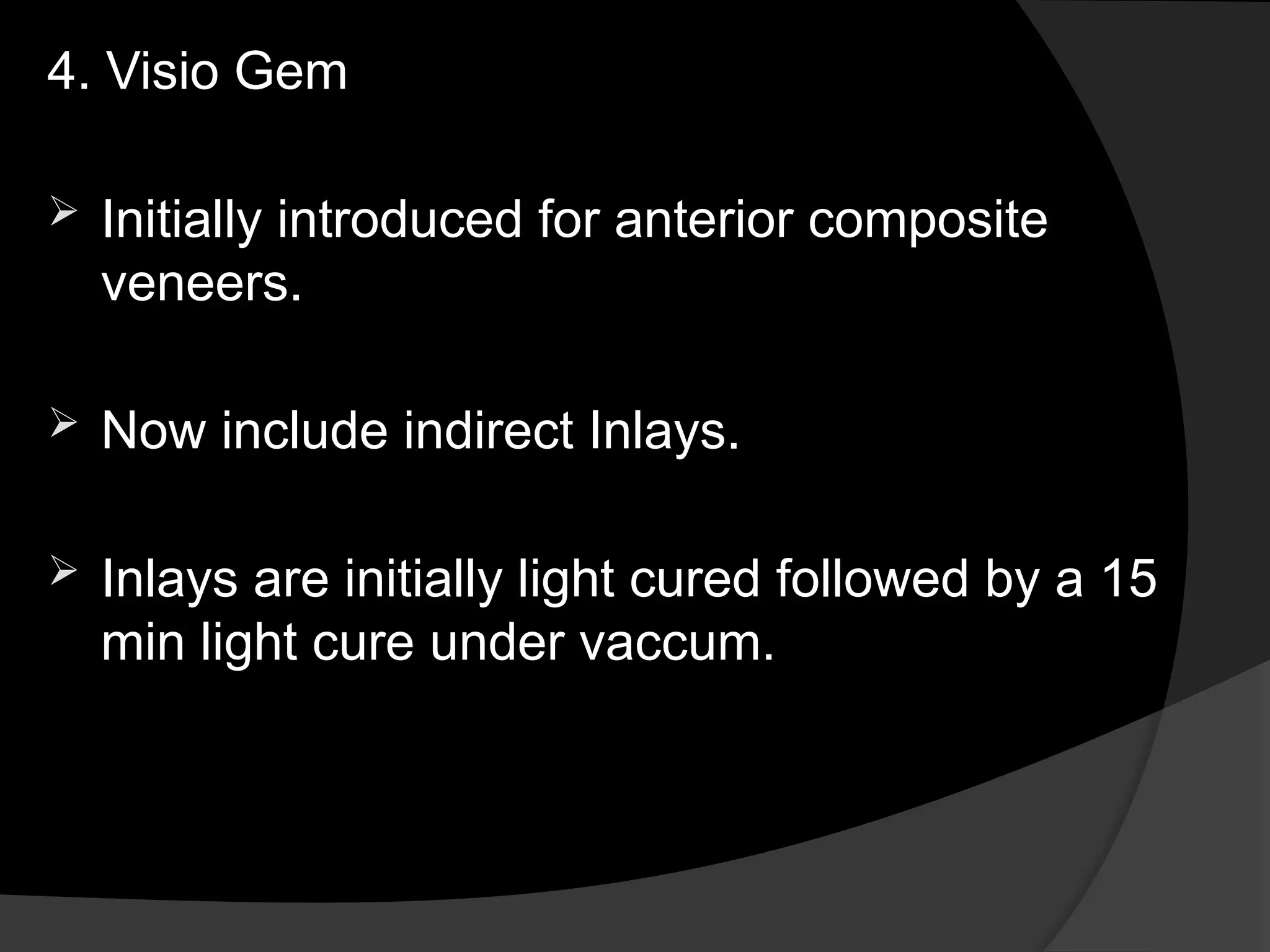
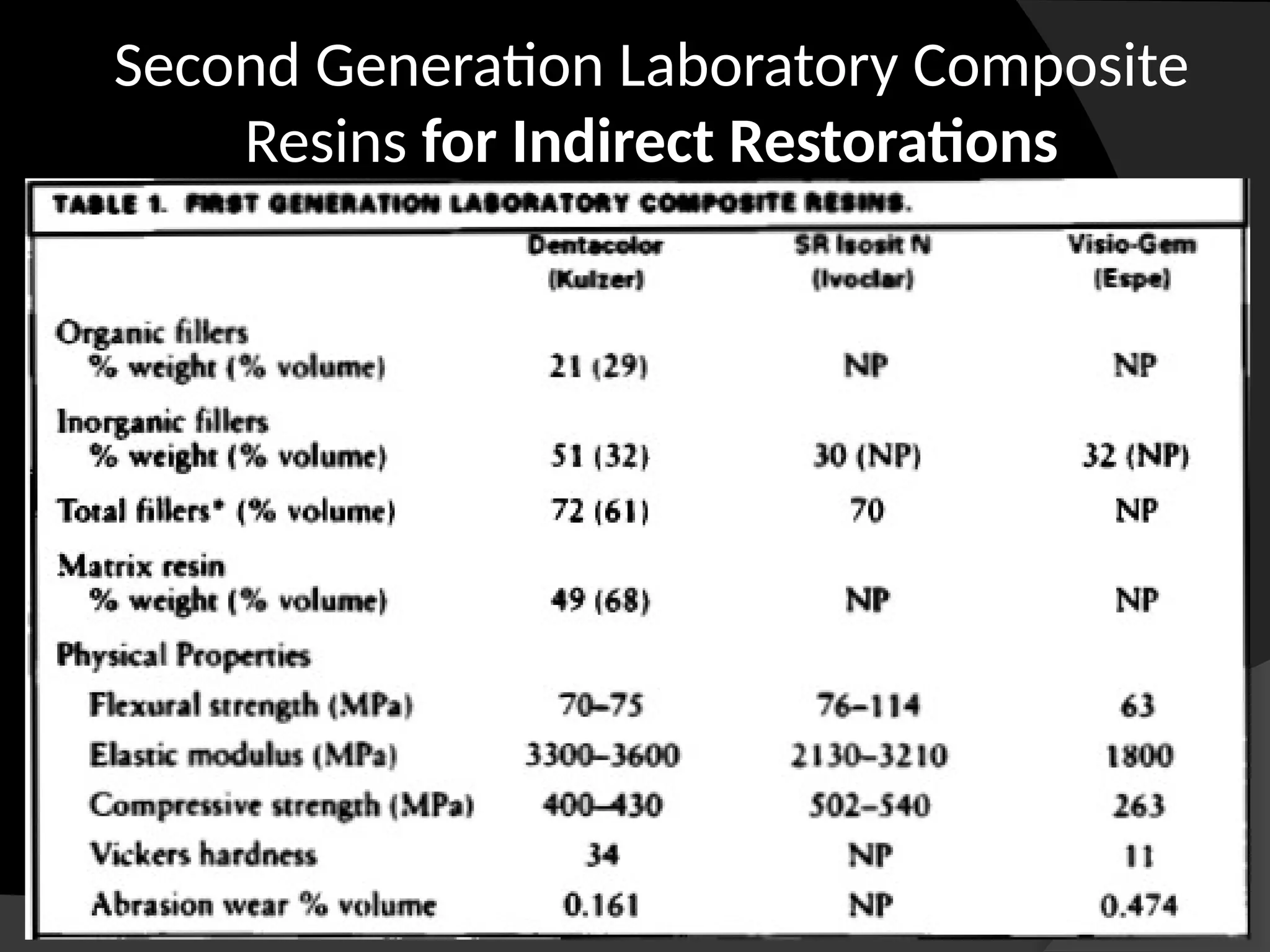
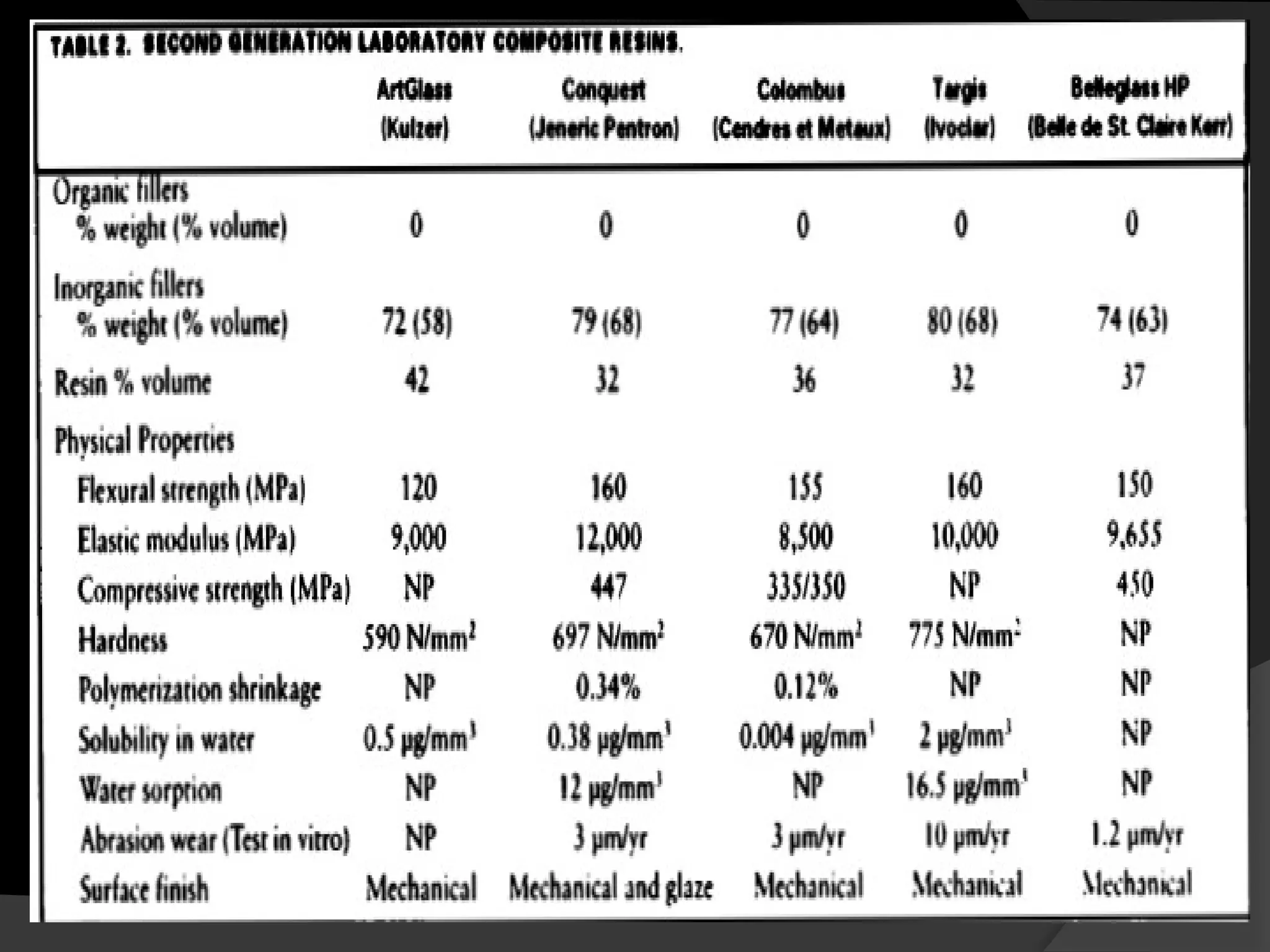
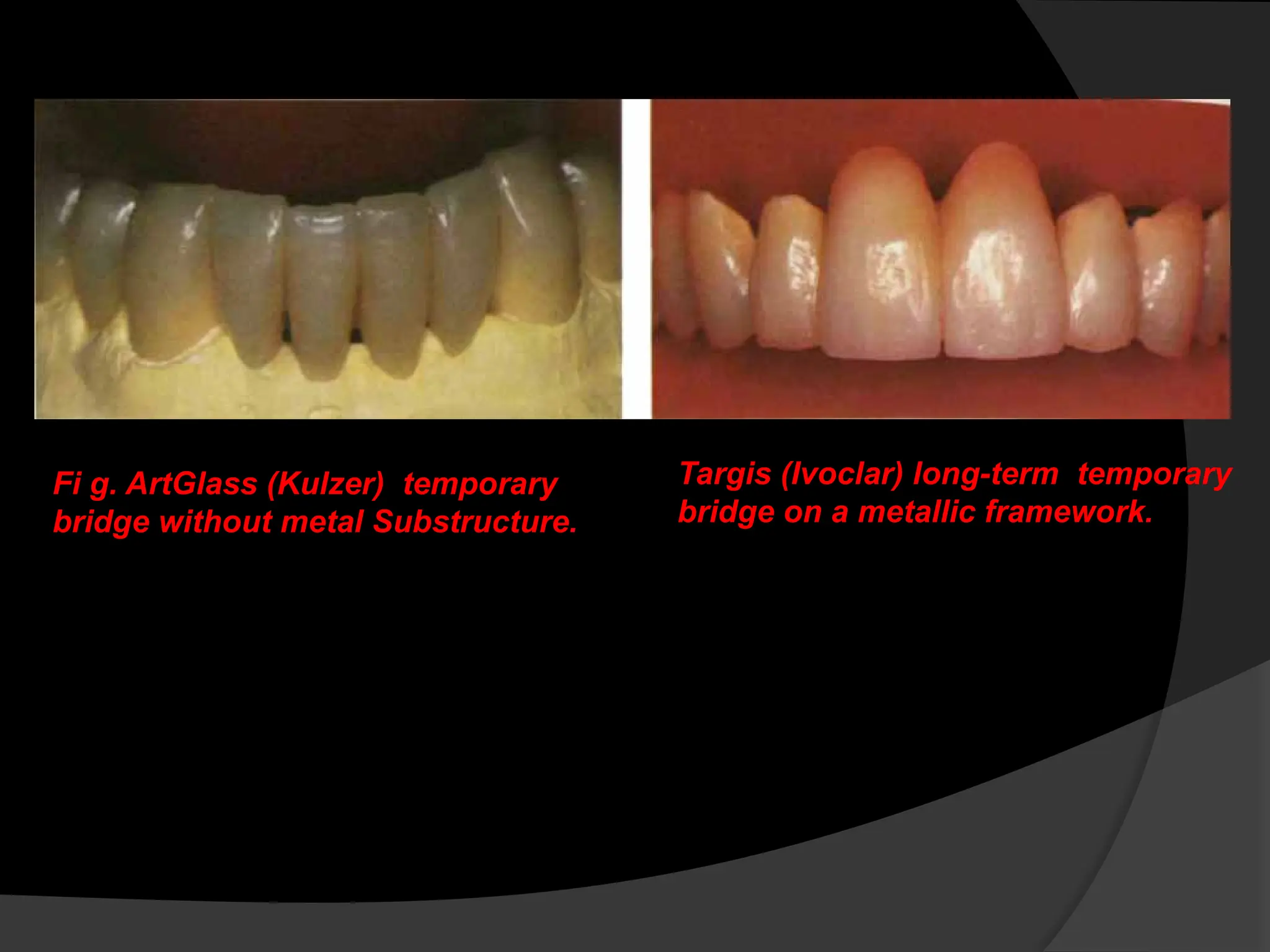
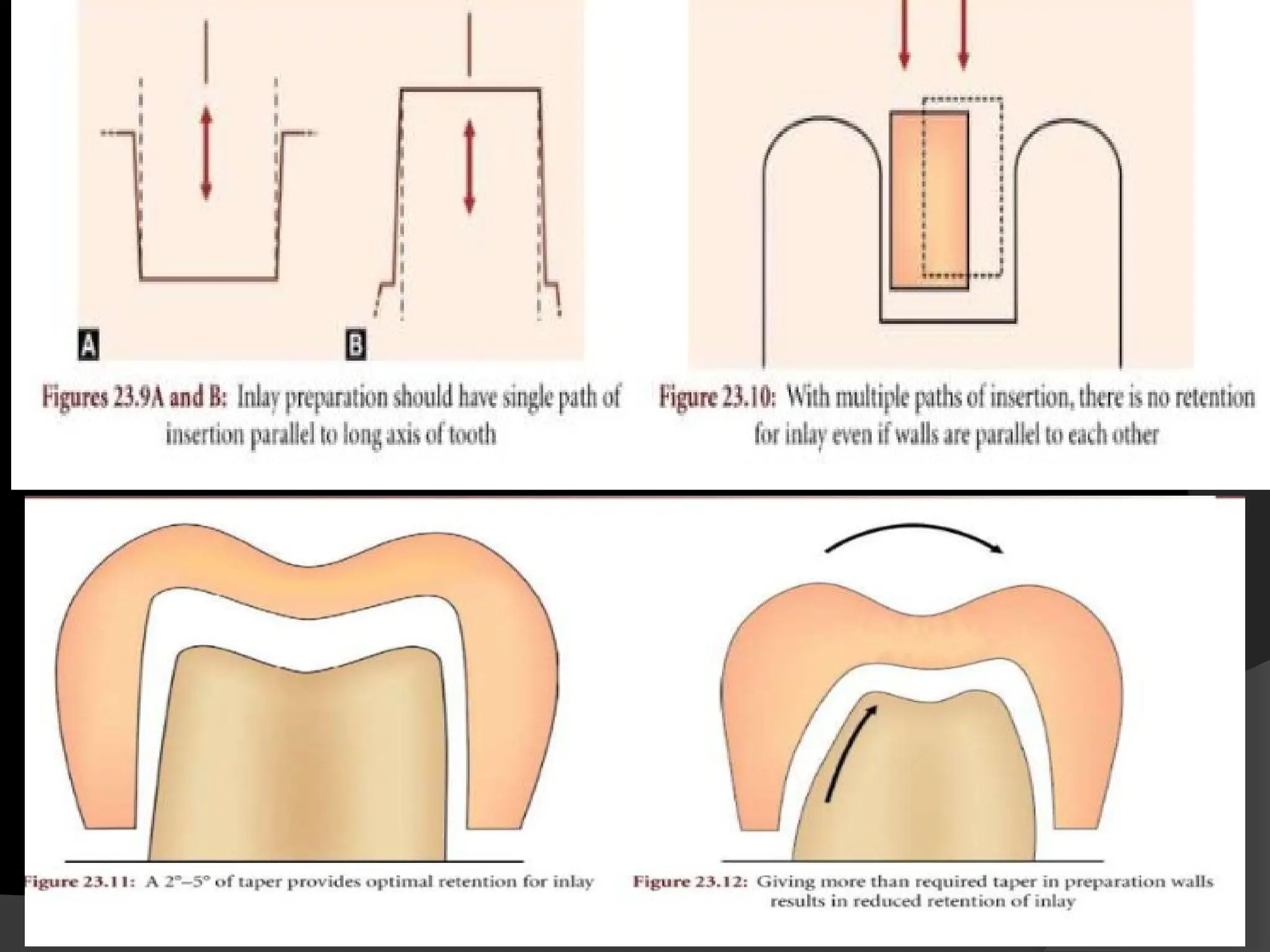
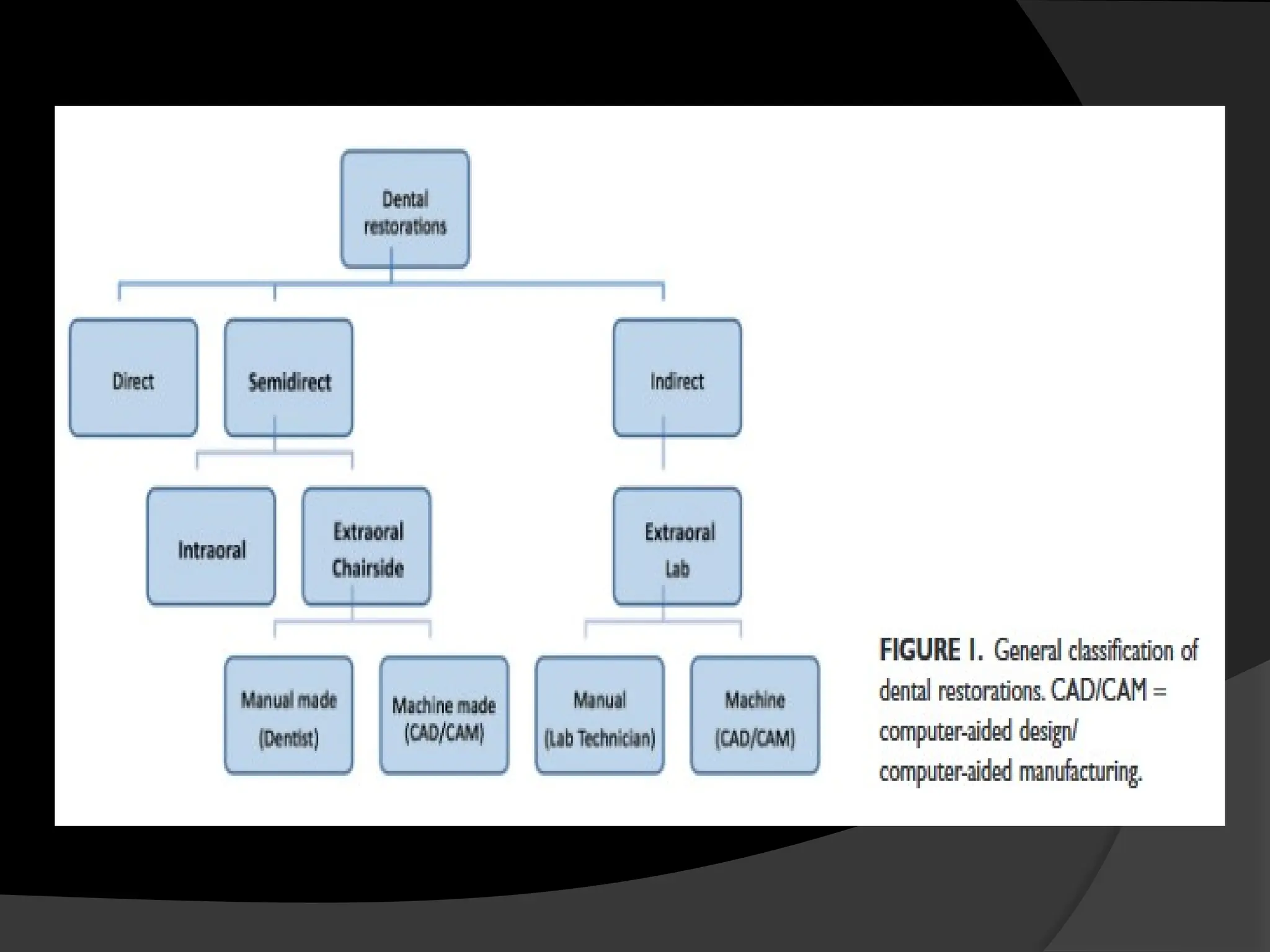
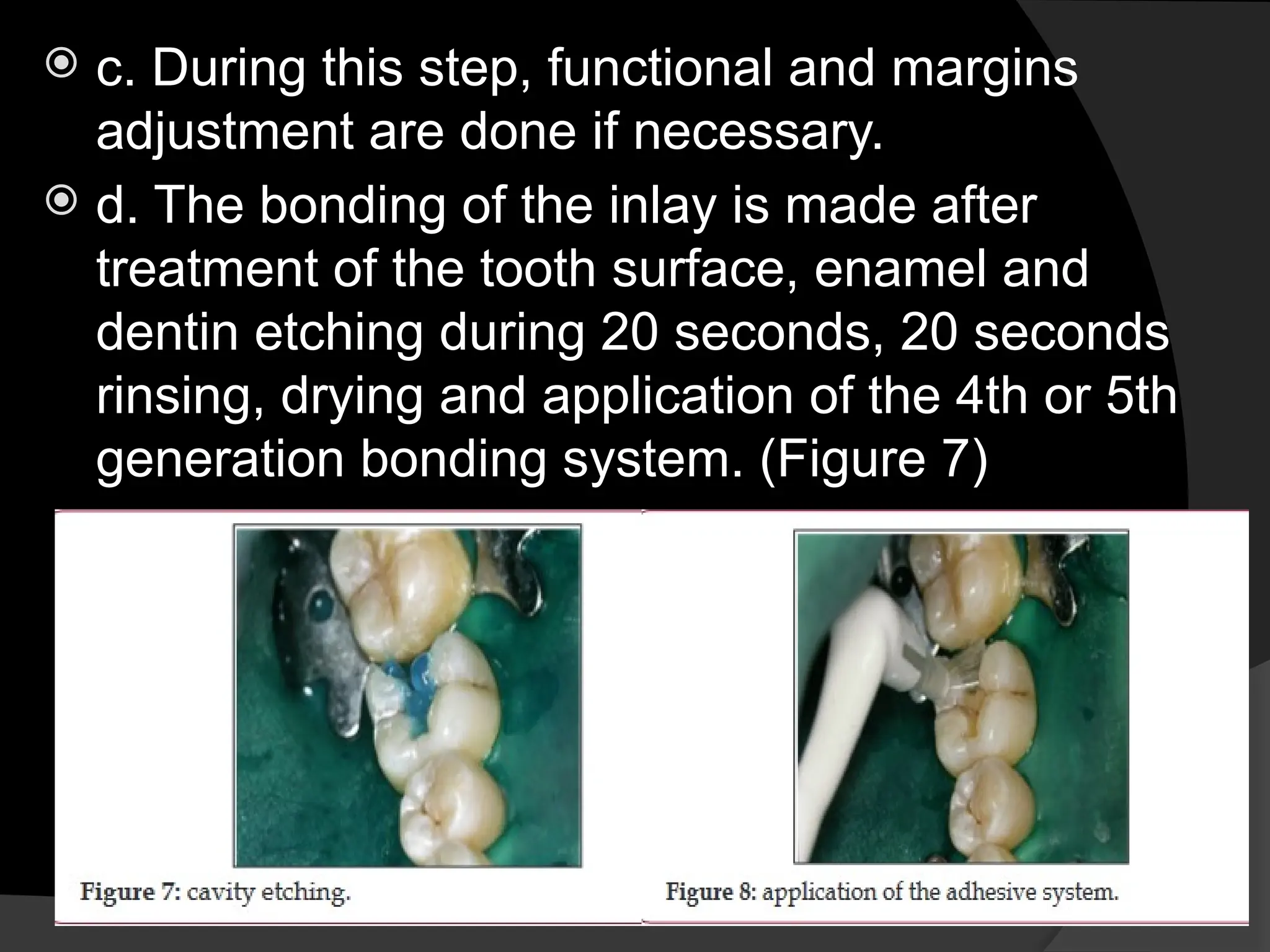
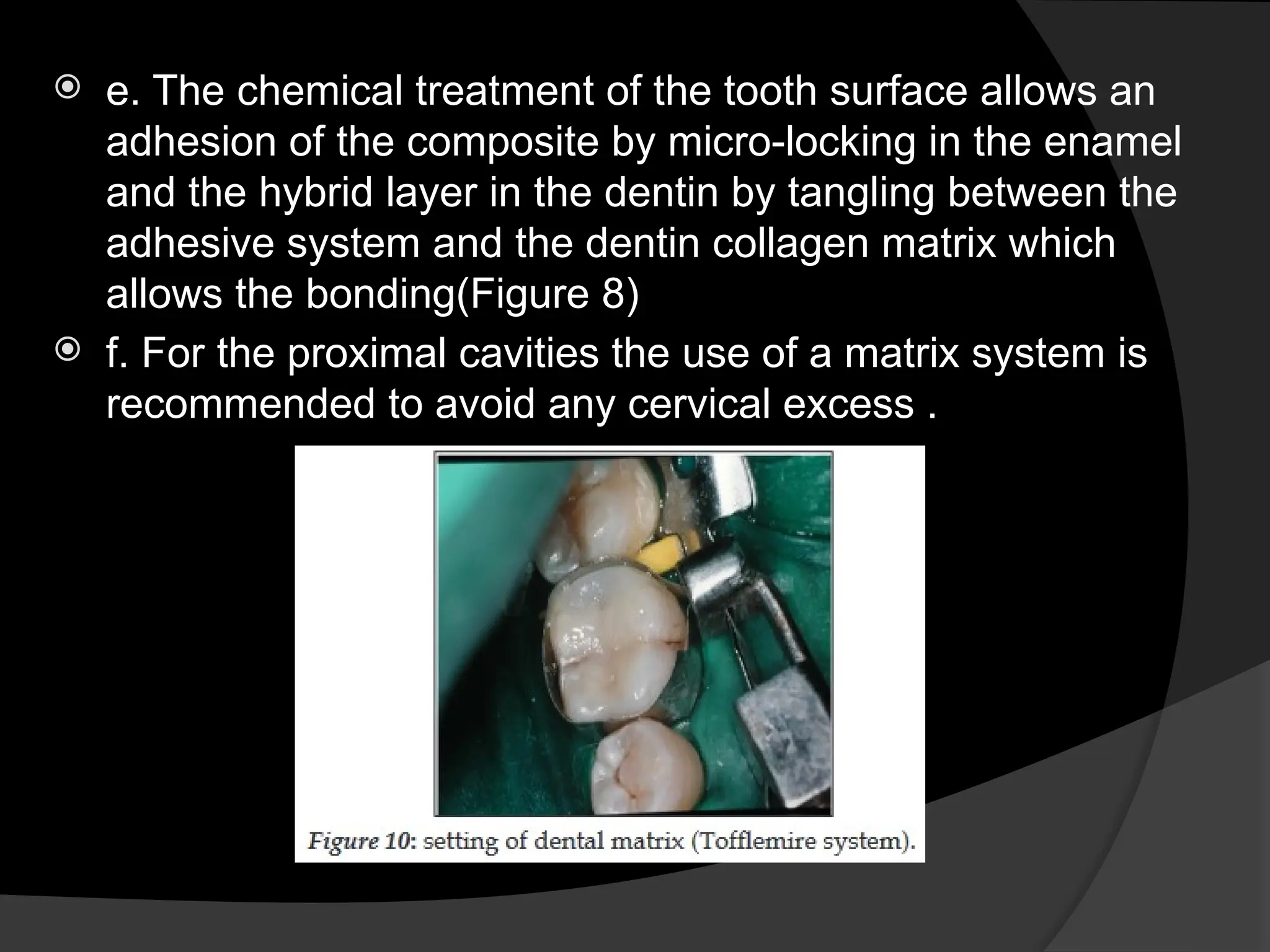
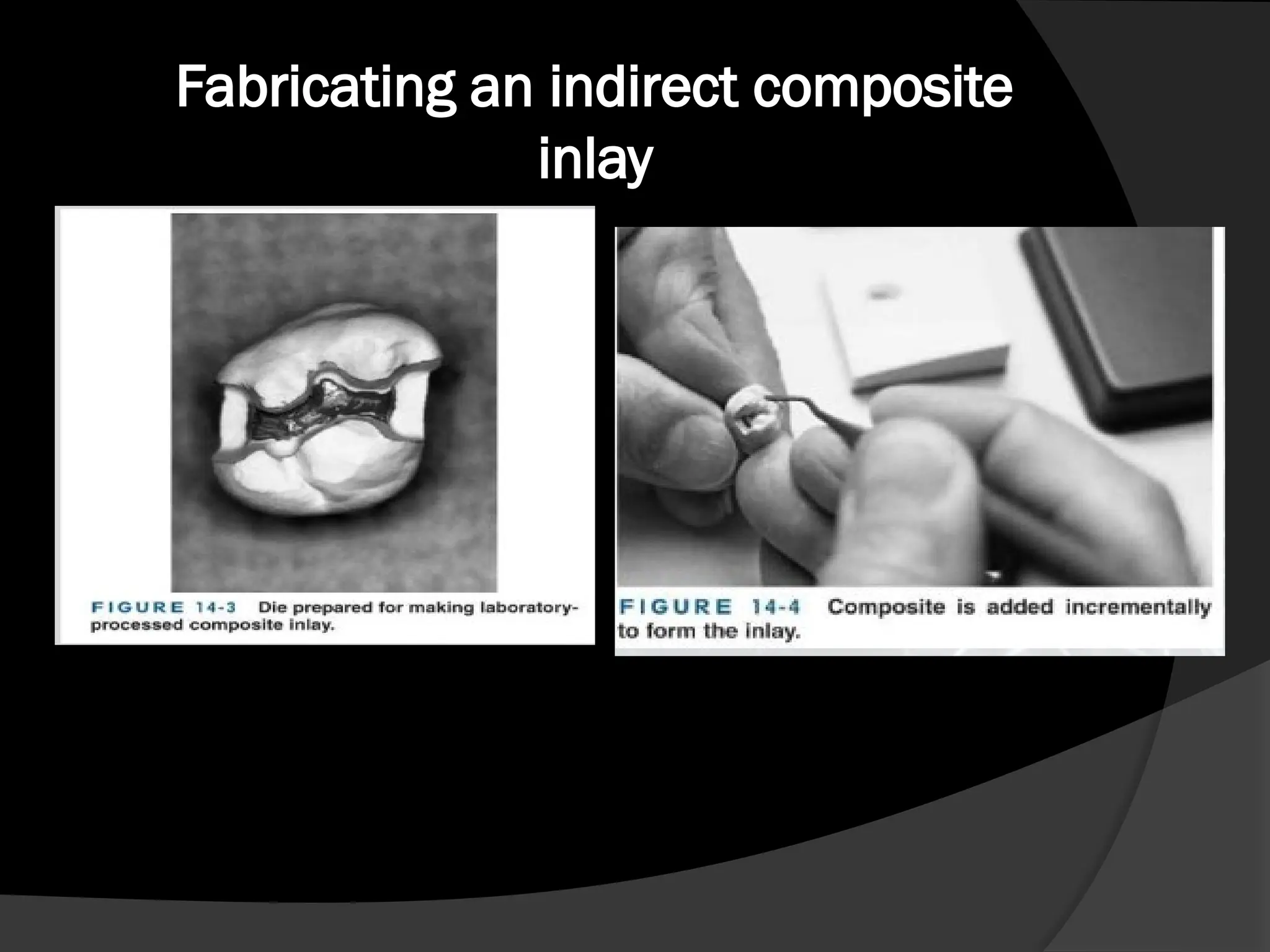
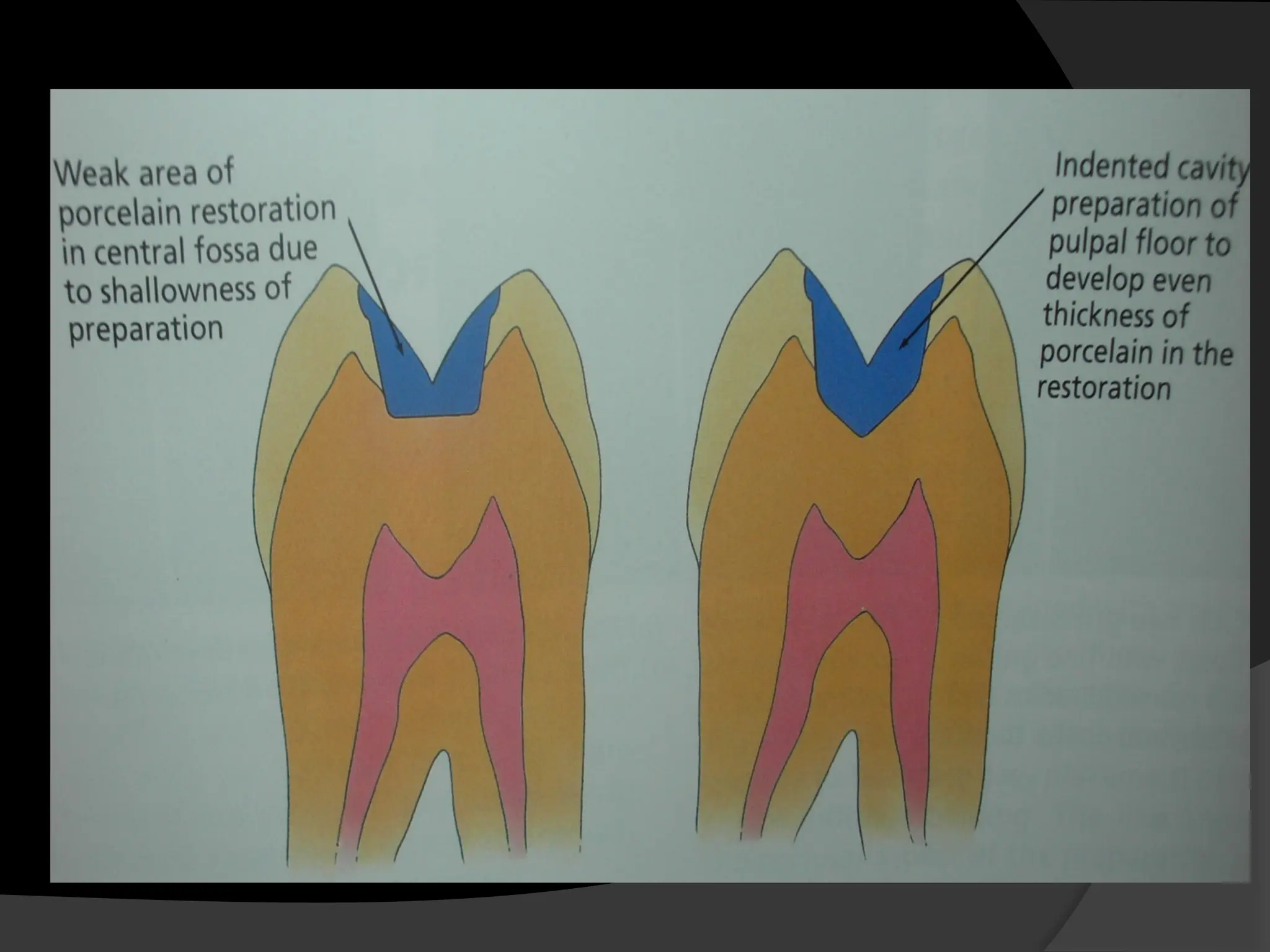
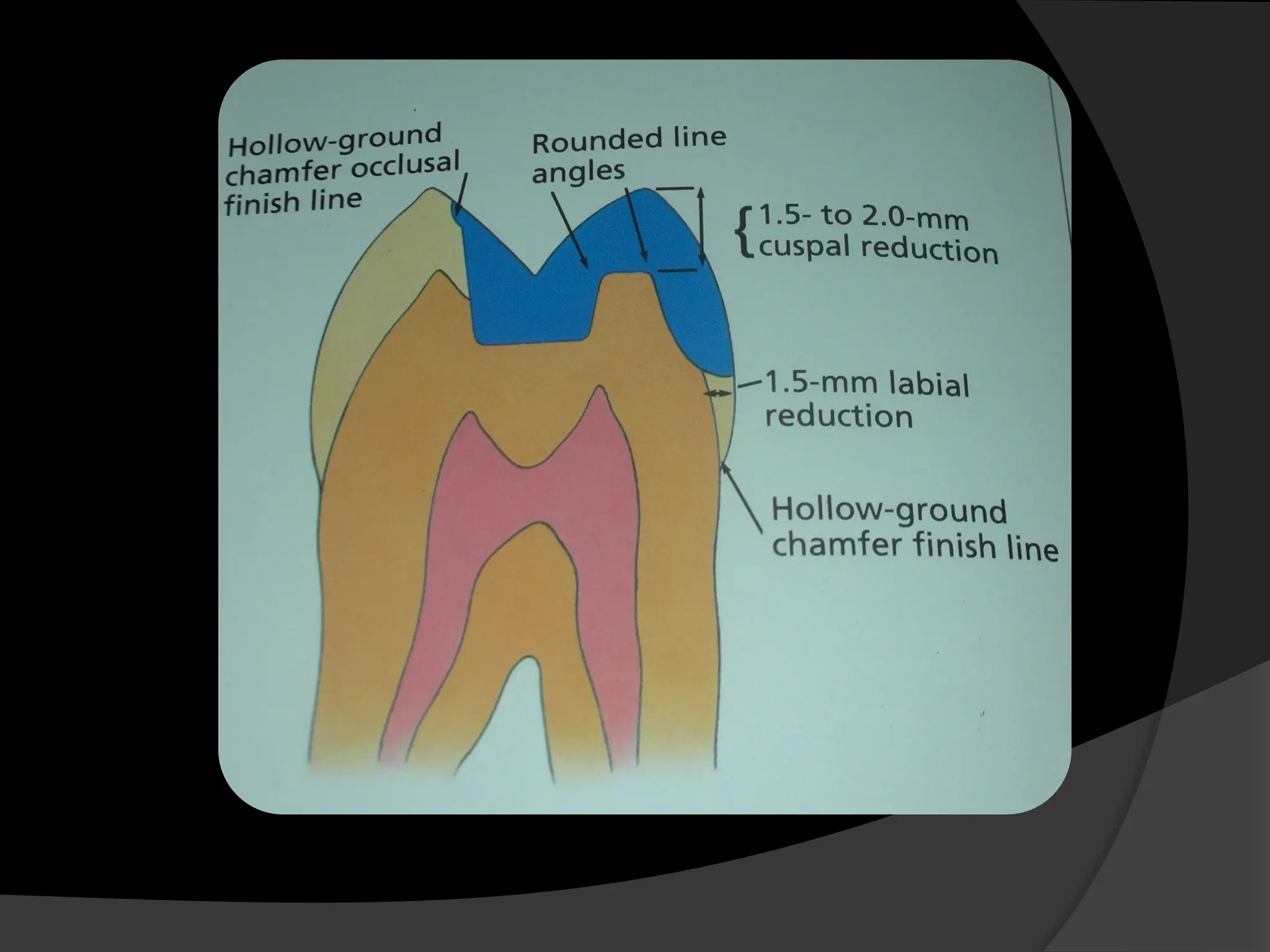
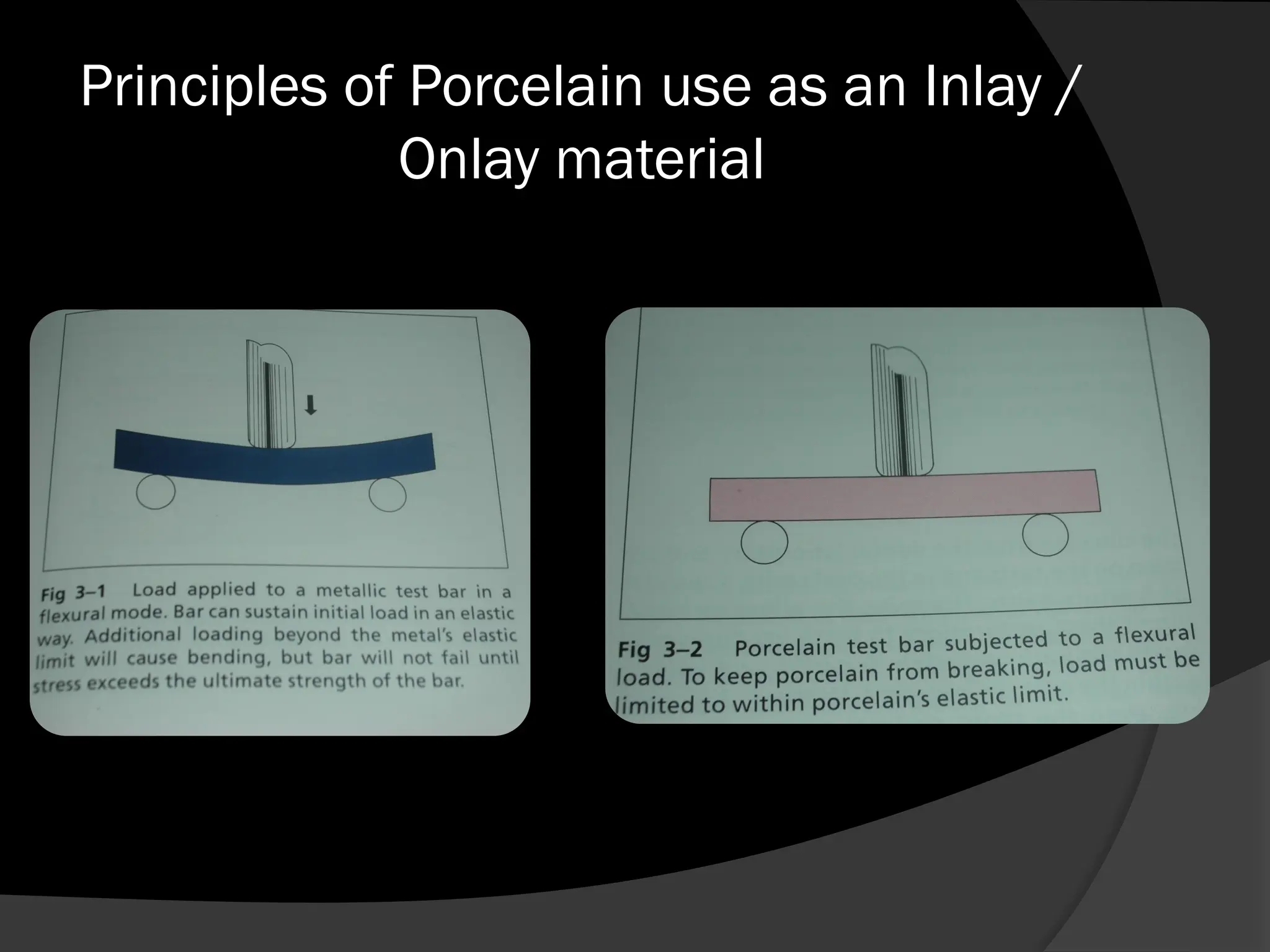
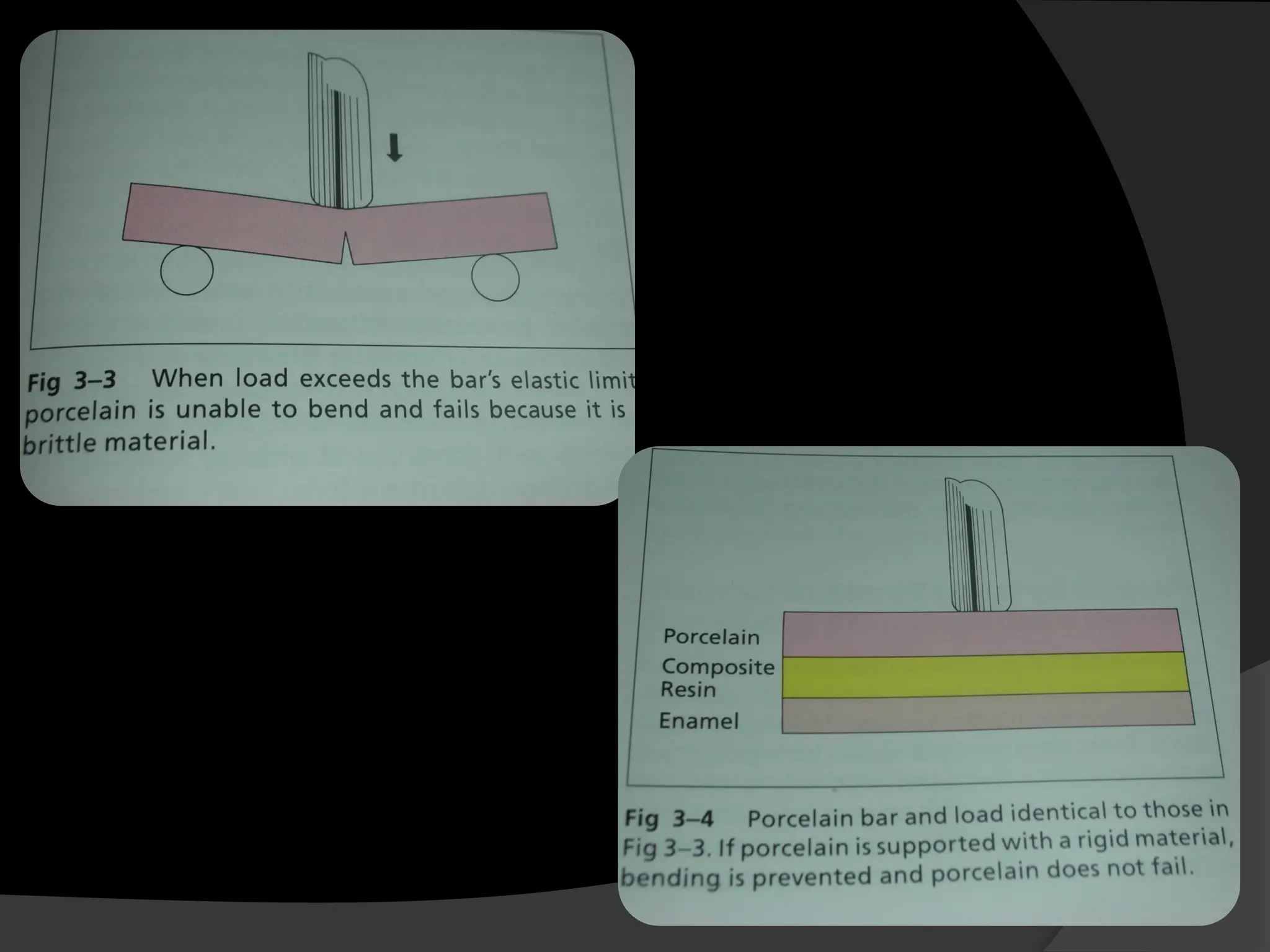
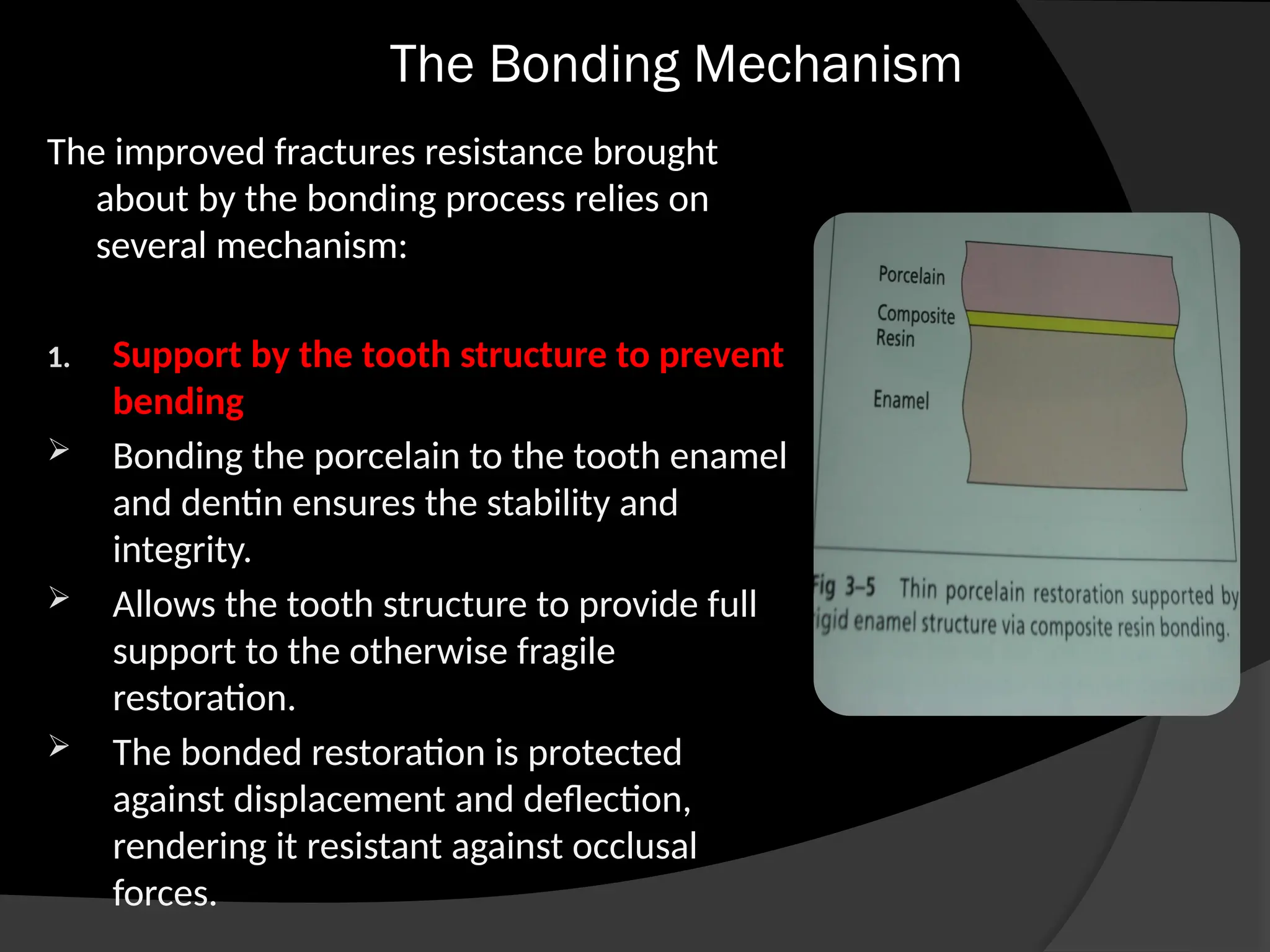
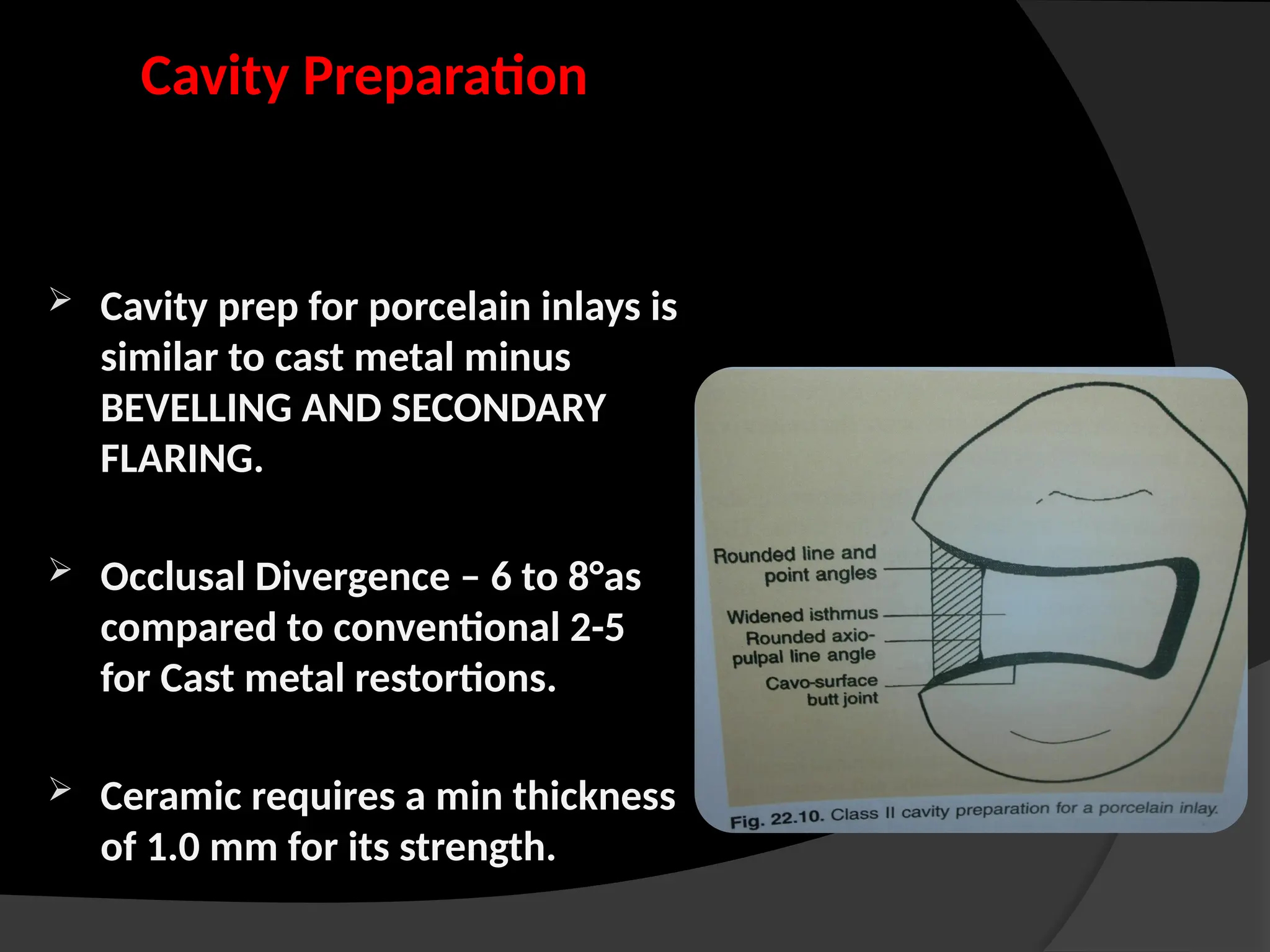
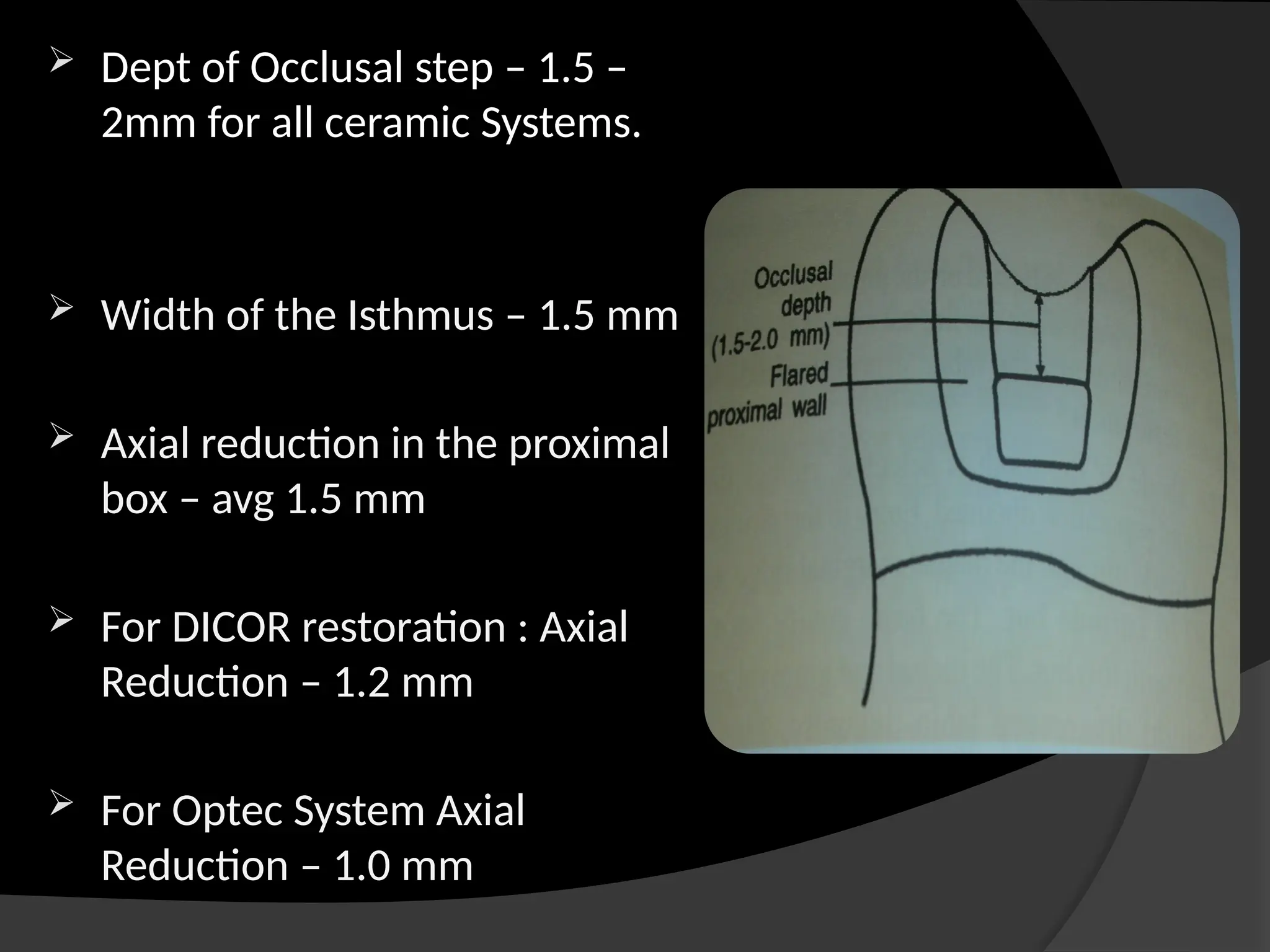
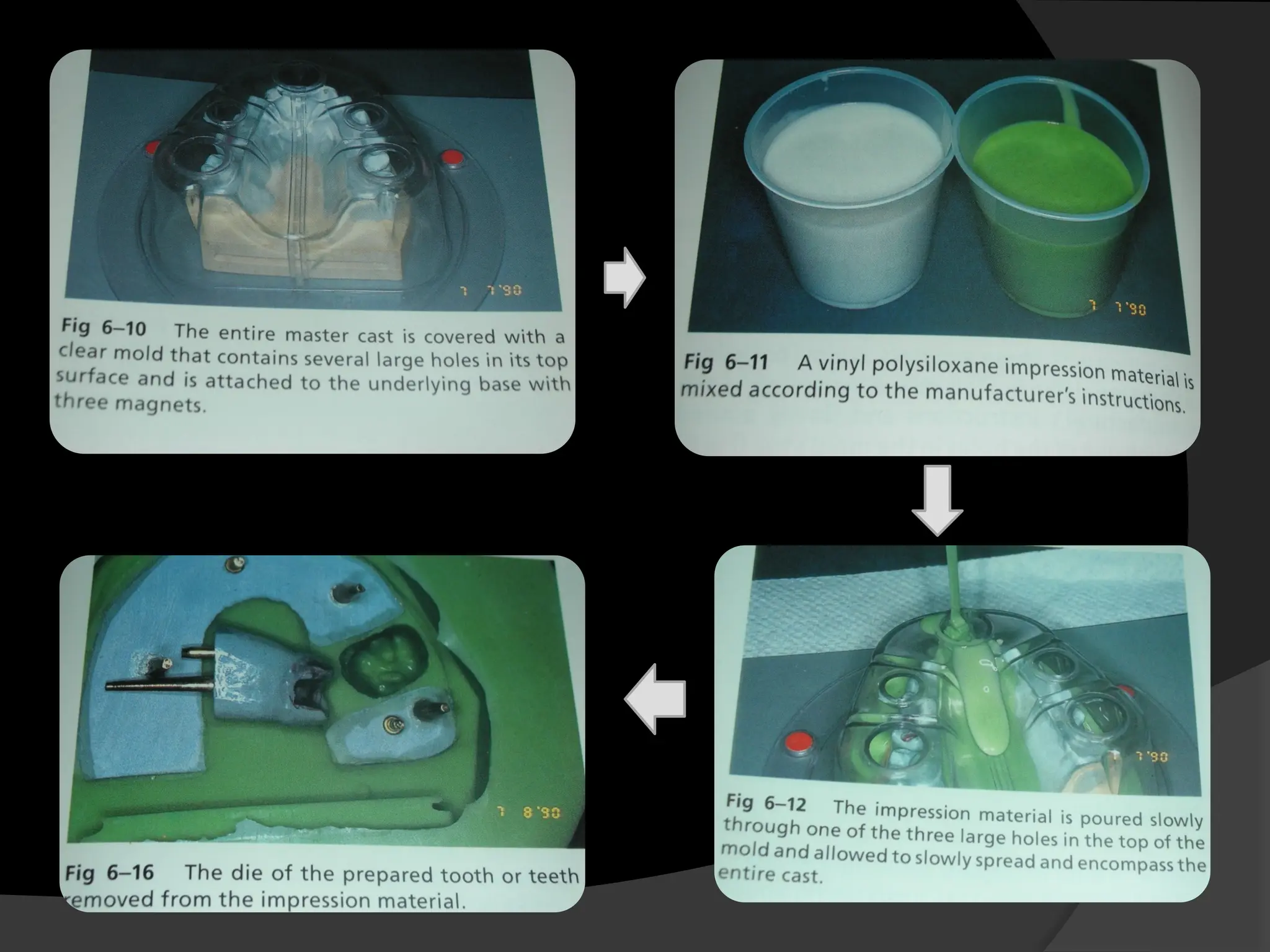
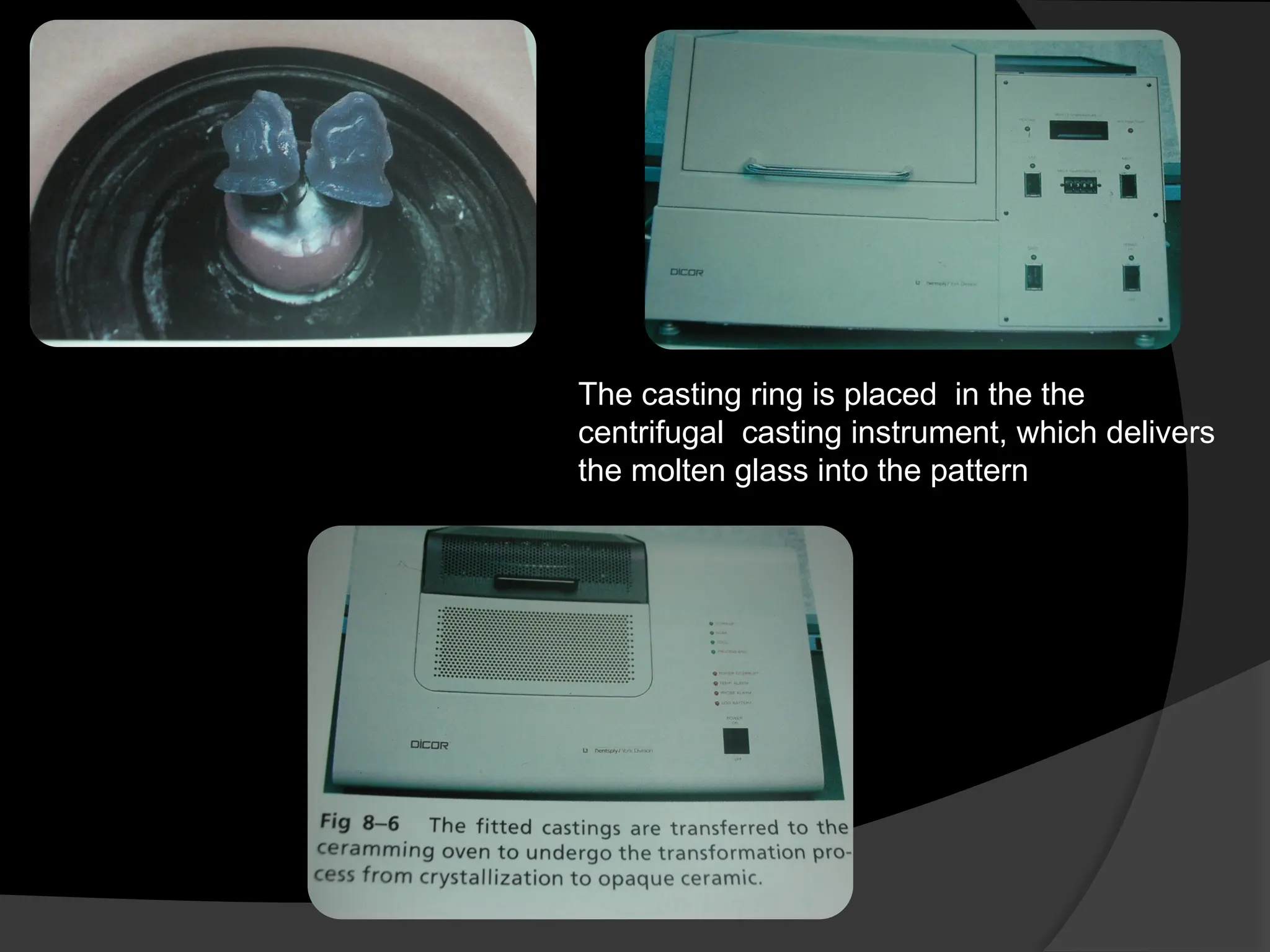
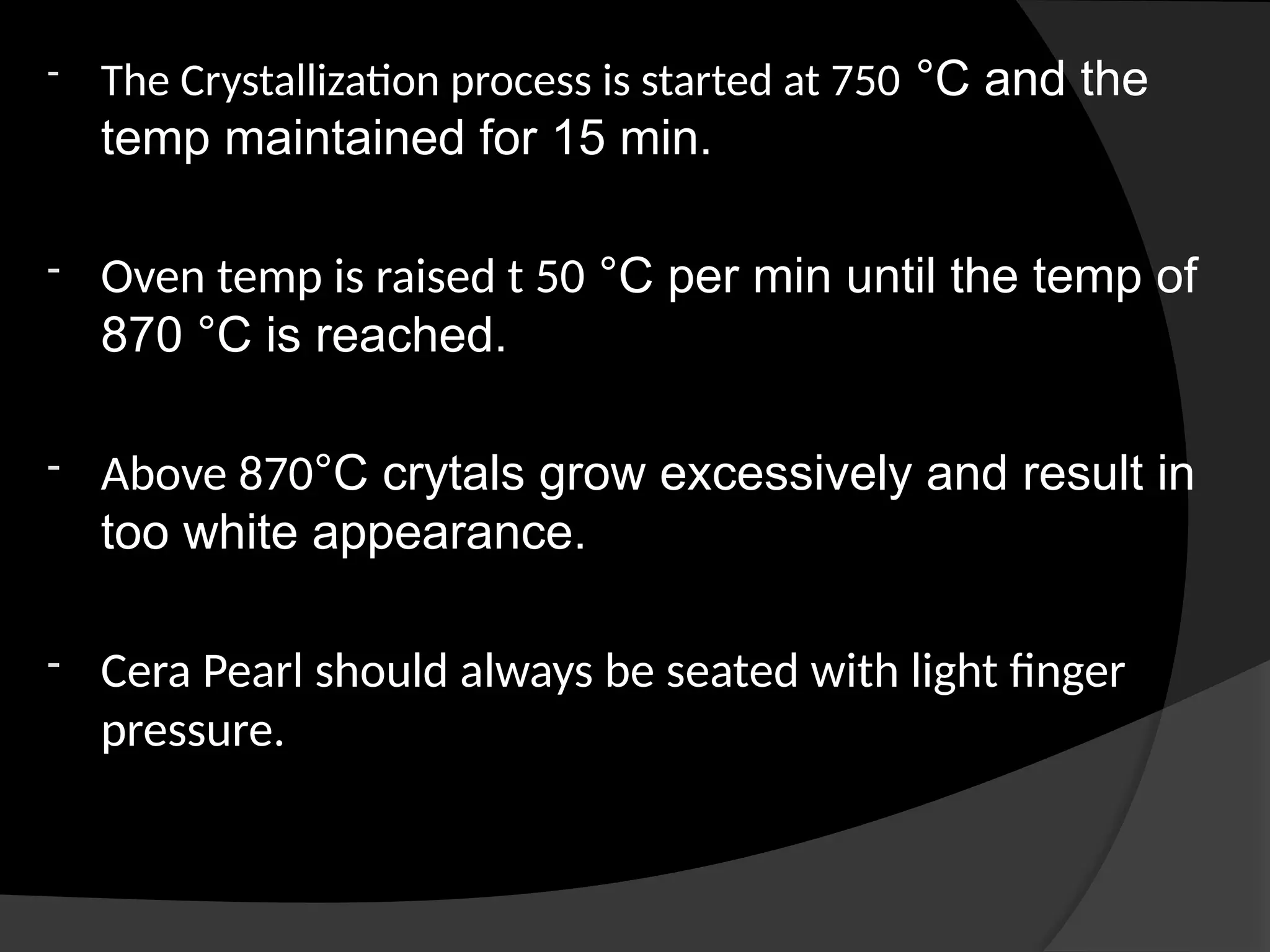
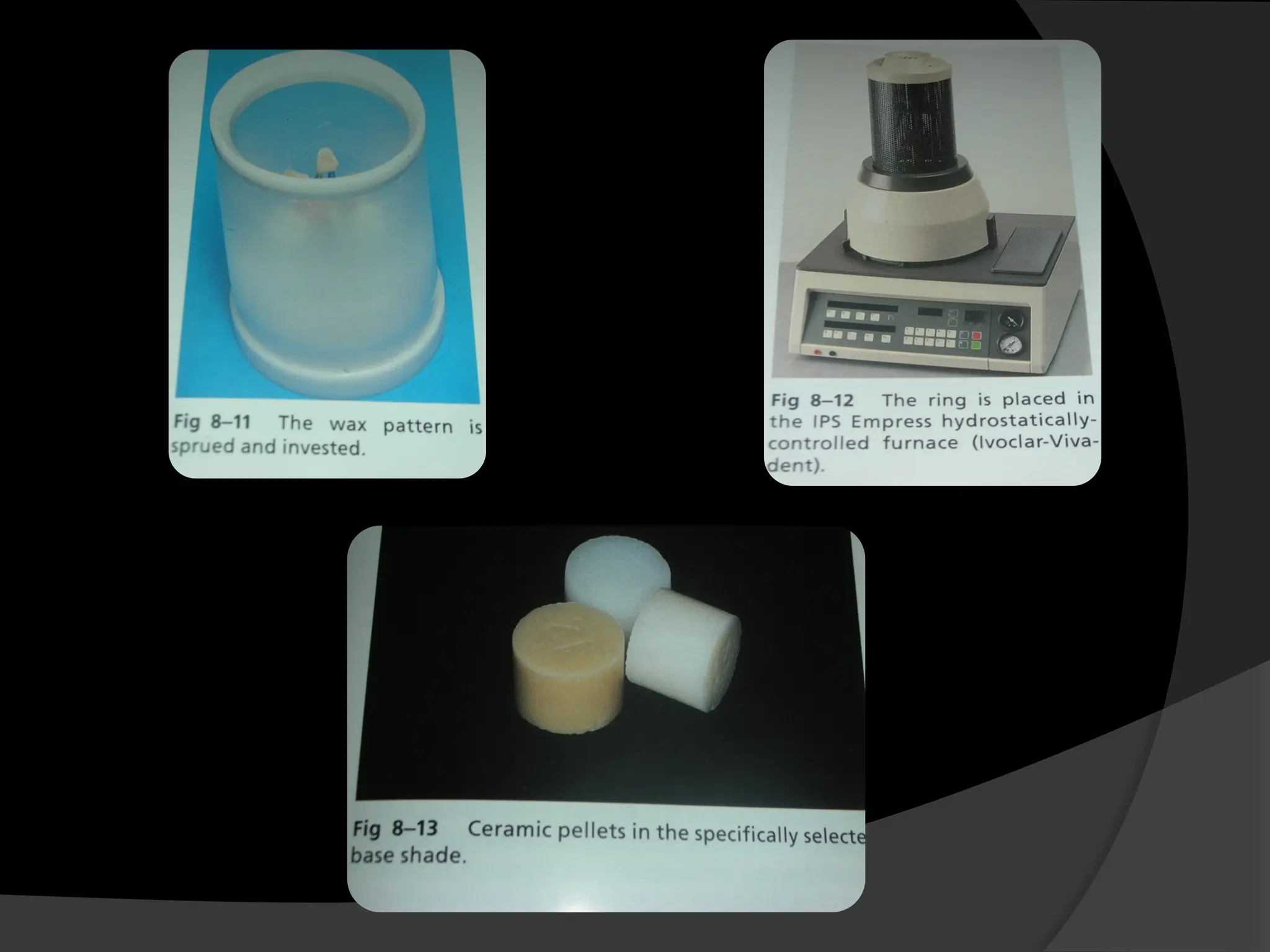
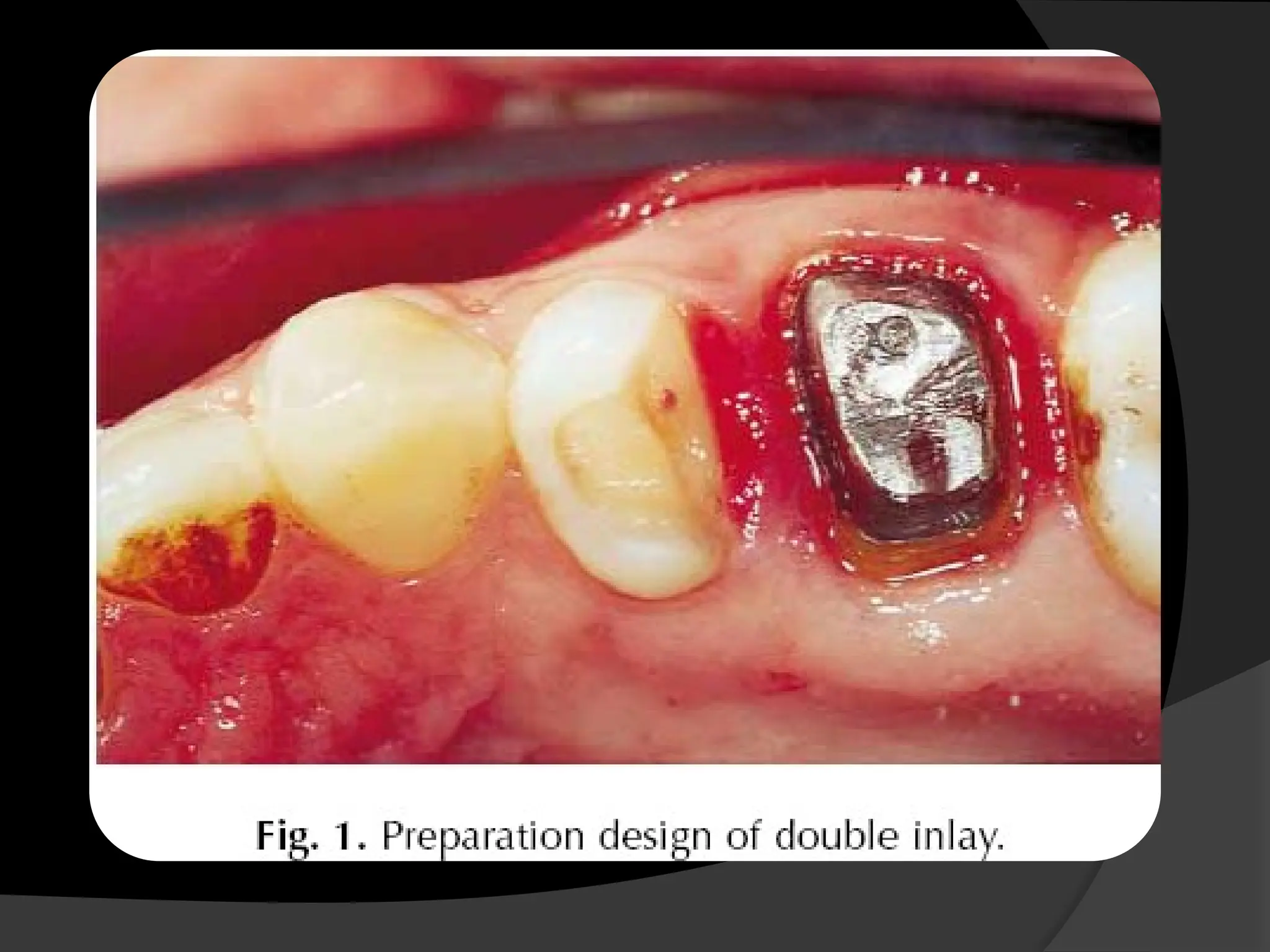
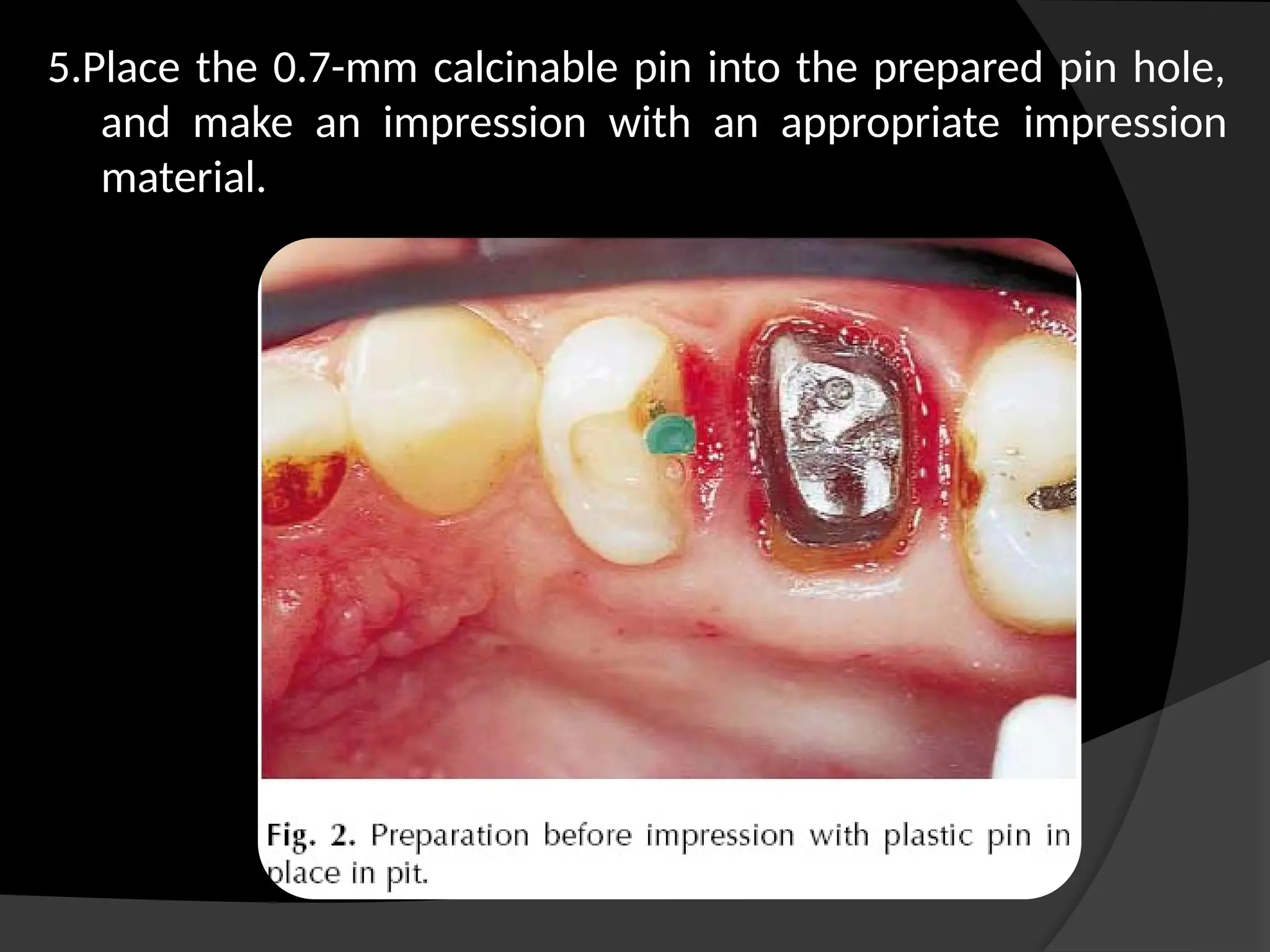
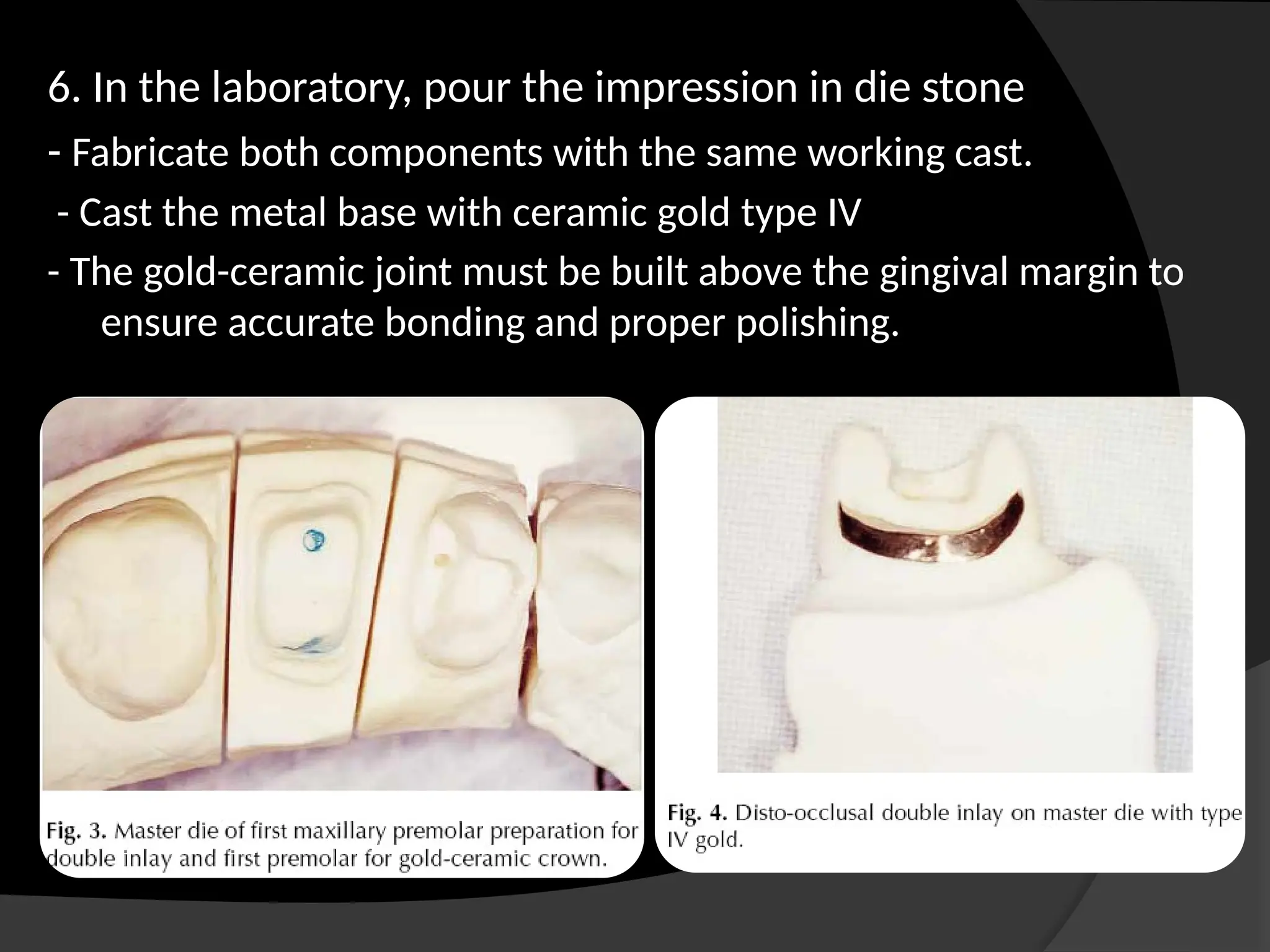
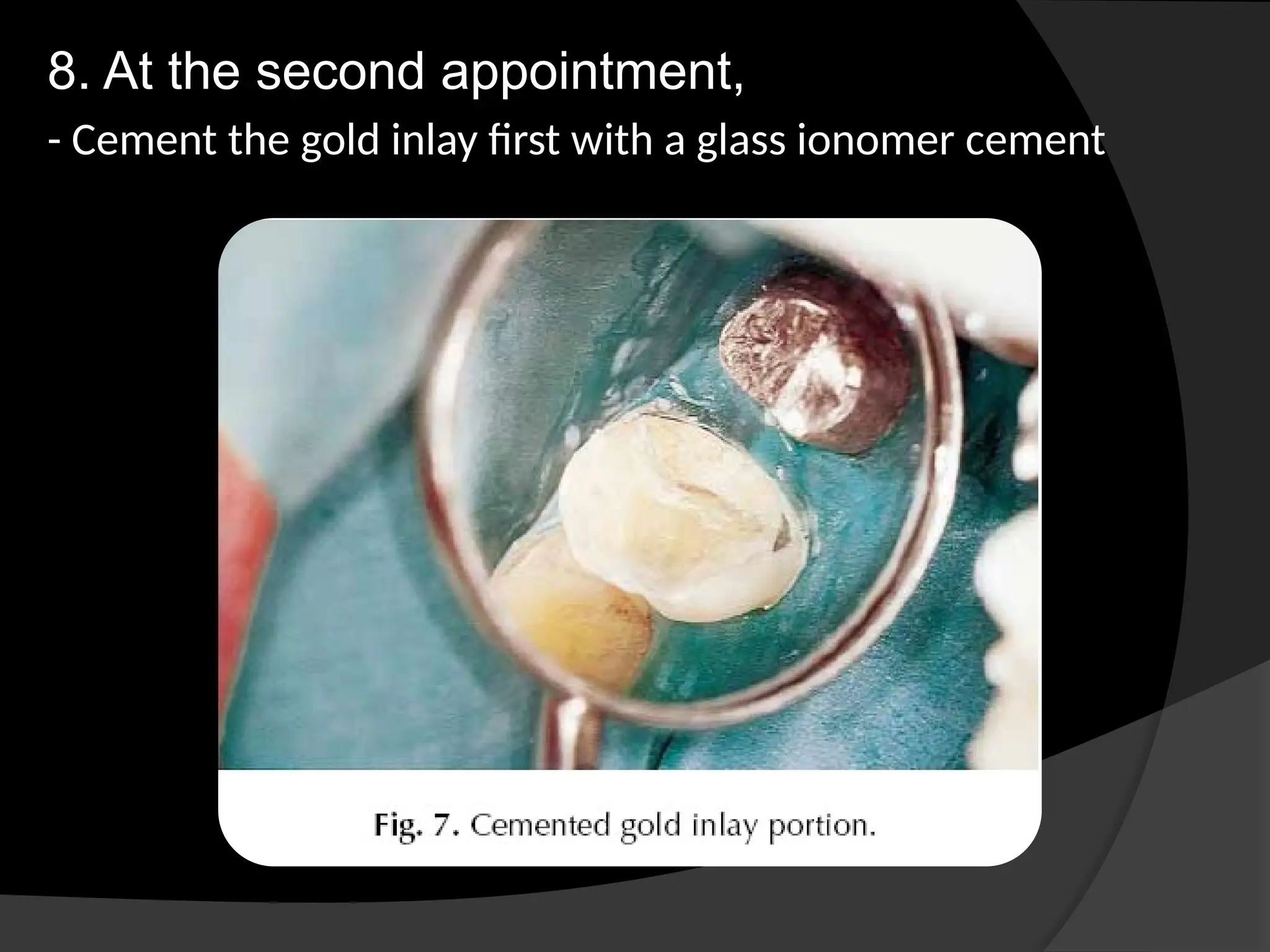
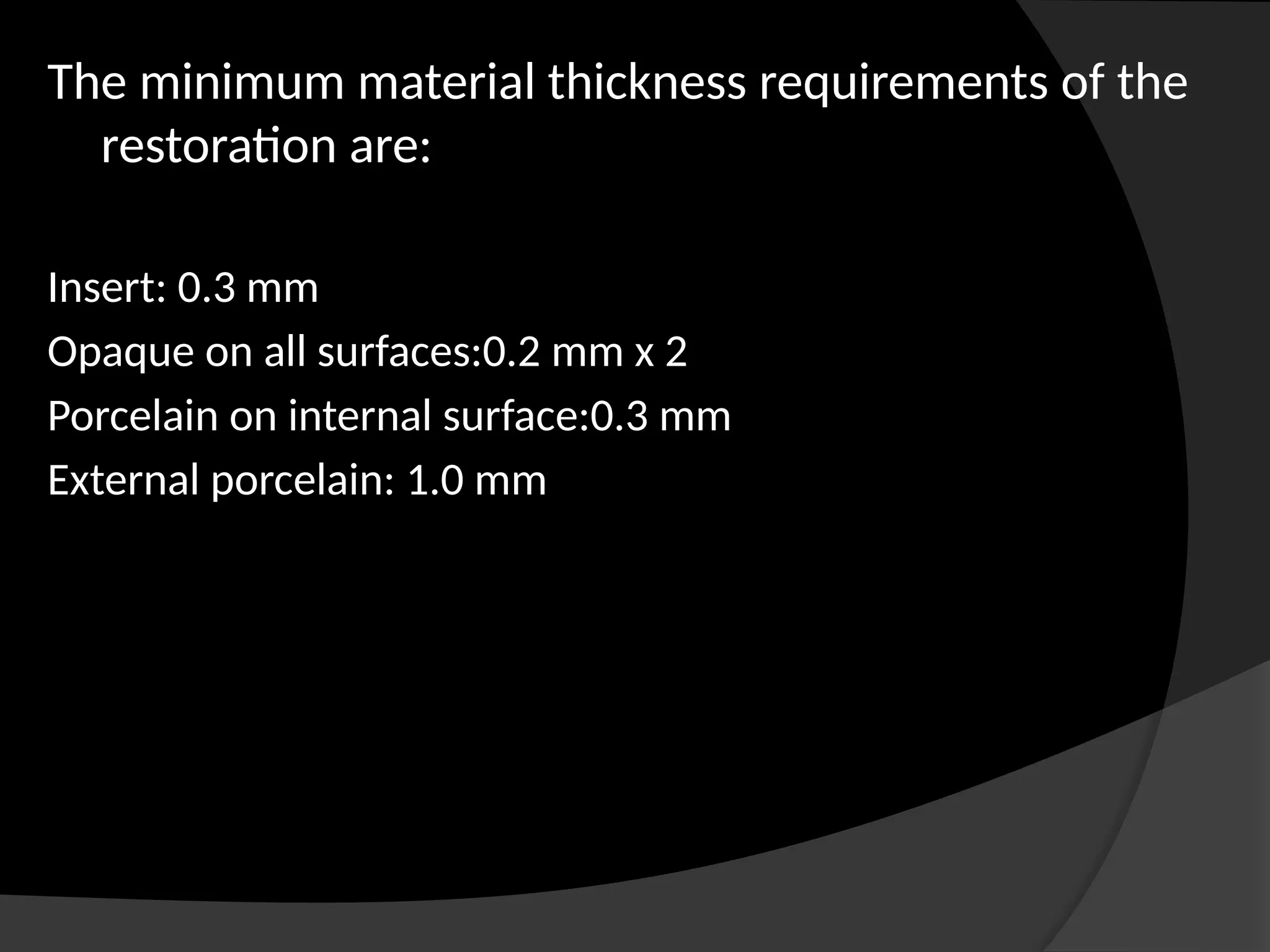
The document discusses the history, advantages, disadvantages, indications, and contraindications of cast restorations, specifically focusing on inlays and onlays. It outlines preparation techniques, retention, resistance principles, and various types of restorations with an emphasis on factors affecting both preparation and material choice. The text also provides insight into porcelain inlays and composite inlays, detailing their development, fabrication methods, and indications for use.