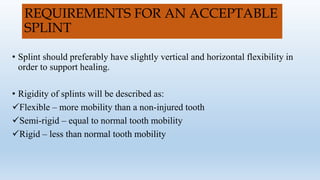
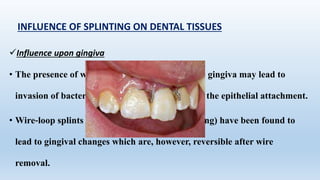
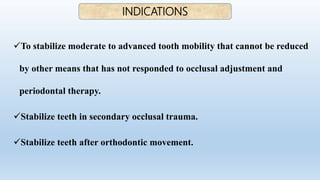
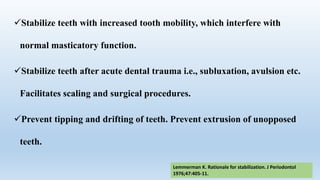
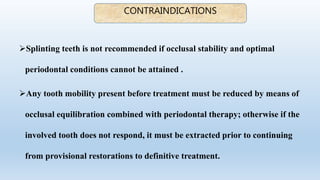
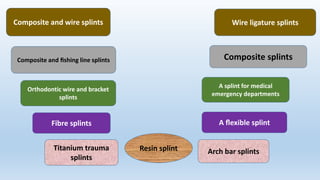
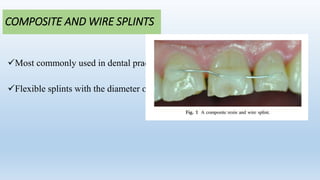
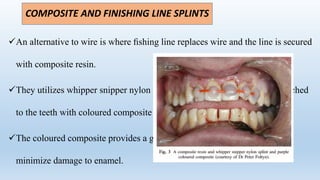
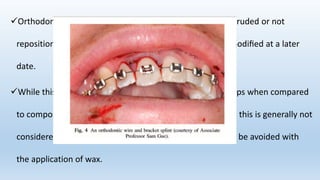
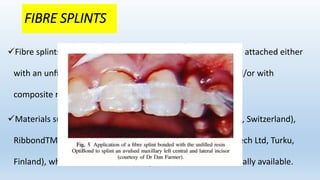
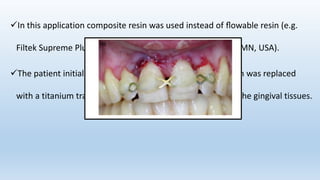
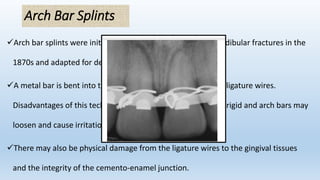
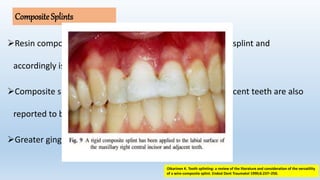
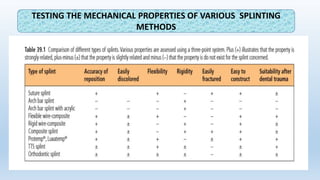
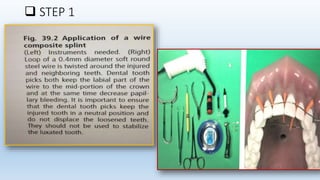
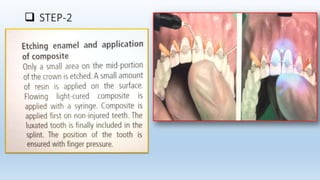
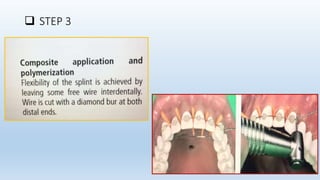
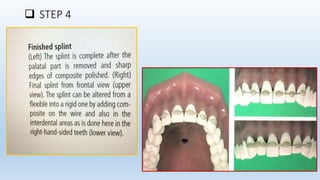
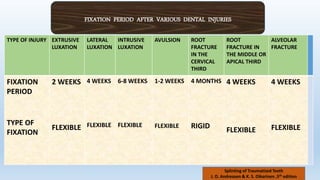
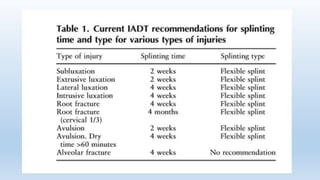
This document discusses splinting of traumatized teeth. It defines splints and their requirements, and describes how splinting influences dental tissues. Different types of splints are described, including composite and wire splints, fibre splints, and titanium trauma splints. Guidelines are provided for splint indications, contraindications, application steps, and recommendations for splint type and duration depending on the specific dental trauma. Factors such as injury classification, healing timeframes, and risk of ankylosis are considered for splint removal timing.