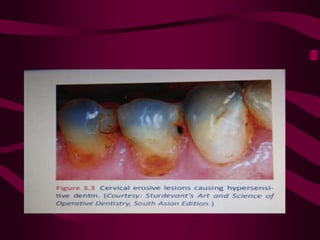
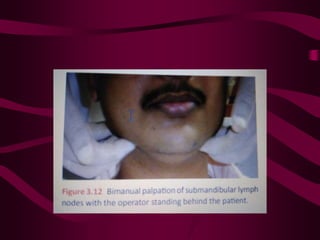
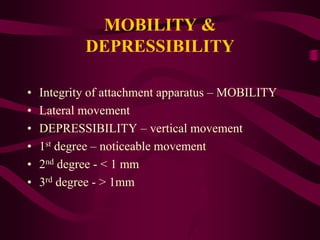
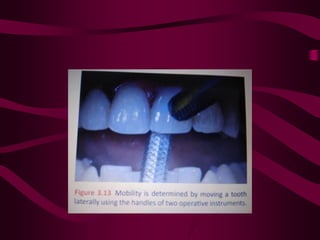
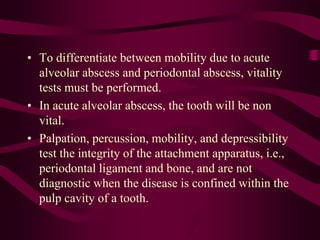
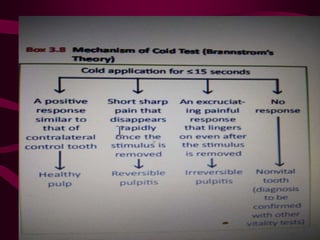
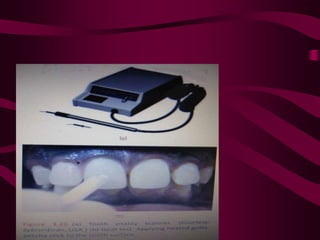
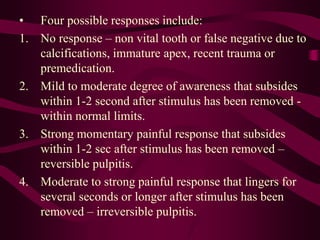
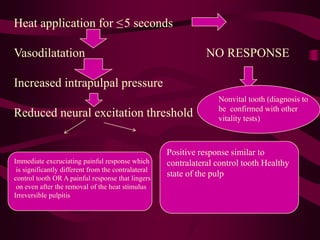
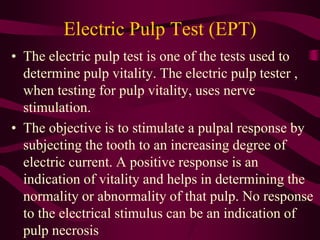
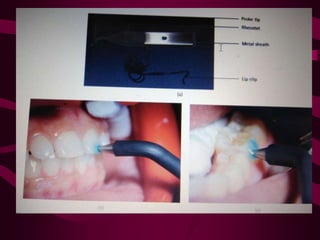
The document outlines clinical diagnostic methods for dentistry, emphasizing the importance of accurate diagnosis based on patient history, chief complaints, and various diagnostic tests. It discusses pain categorization, symptoms, and specific methods for assessing pulp vitality and dental conditions, including thermal testing, electric pulp testing, and advanced imaging techniques like cone beam computed tomography (CBCT). The document also details the diagnostic process involving visual inspection, percussion, palpation, mobility testing, and radiography to ensure effective diagnosis and treatment in endodontics.