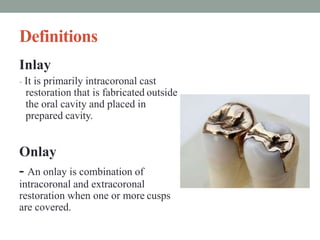
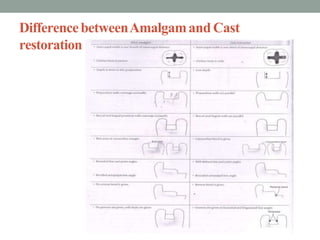
This document provides information on cavity preparation for cast metal restorations. It discusses various types of cast restorations like inlays and onlays. Key points include:
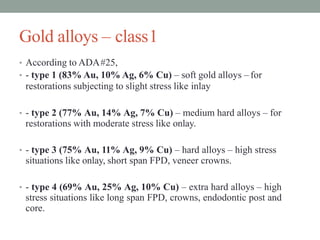
- Different classes of casting alloys are described based on their composition, such as gold-based, low gold, non-gold platinum and nickel-chromium alloys.
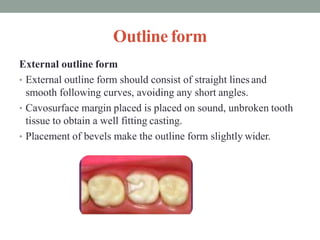
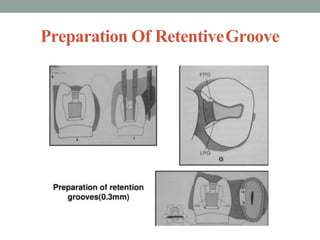
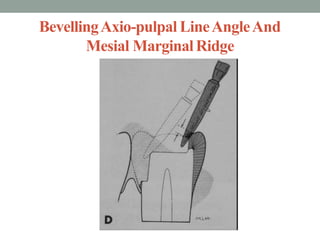
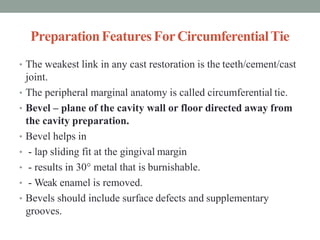
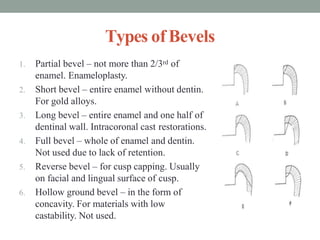
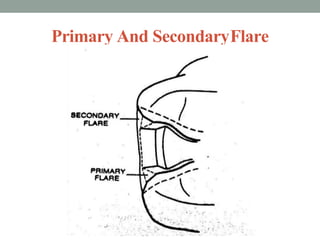
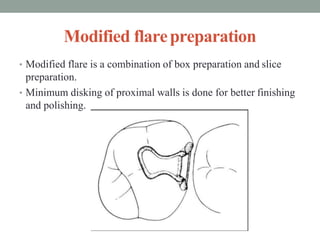
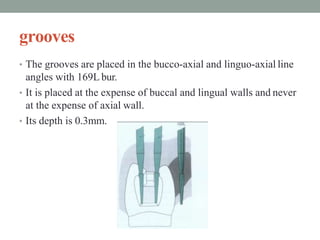
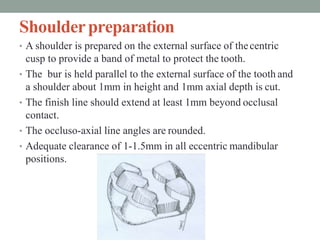
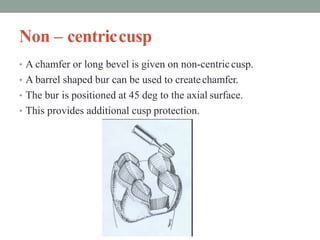
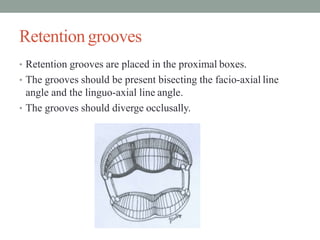
- Principles of cavity preparation include following tooth anatomy, maintaining resistance and retention forms, and preparing cavities with resistance and retention features like dovetails.
- Specific burs and techniques are outlined for preparing cavities in molars and premolars, including maintaining proper cavity depth, taper, and finishing line placement.