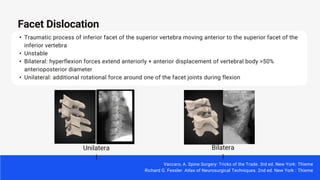
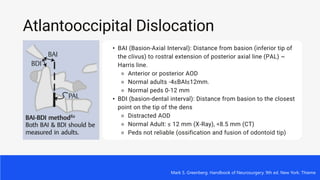
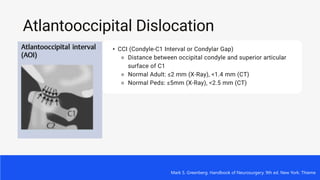
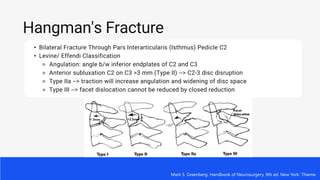
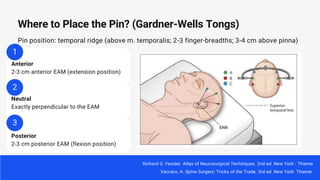
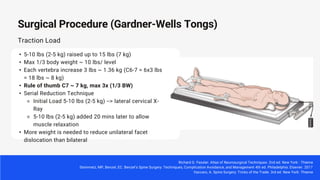
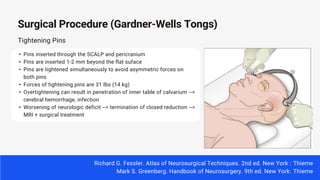
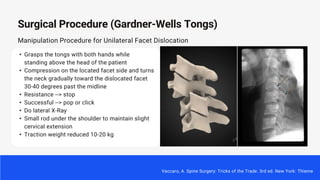
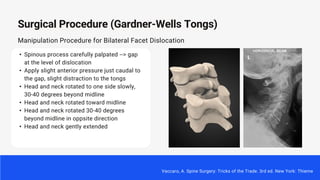
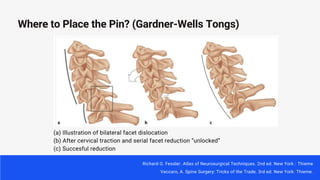
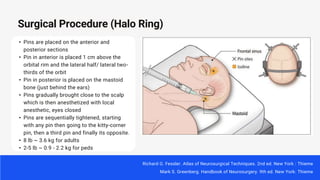
This document discusses cervical traction techniques for reducing cervical spine fractures and dislocations. It begins with an overview of the indications and advantages of cervical traction, including reducing fracture-dislocations to decompress the spinal cord. Two common devices for cervical traction are described - Gardner-Wells tongs and halo rings. Placement of pins and weights used are outlined for safe and effective closed reduction. Common fractures like facet dislocations and Hangman's fractures are also reviewed.

















![• Patients typically receive traction for 3–8 weeks
at 30%– 50% of their BW
• Traction weight was based on BW (kg) and
etiology, represented as
%BW: ([traction weight/BW] × 100%)
• One to two pounds (0.45–0.91 kg) of weight
was added daily until goal %BW was achieved
• The mean absolute correction for kyphosis
deformity was 35° ± 16.3° (range 18°–68°)
How Long?
Verhofste BP, Glotzbecker MP, Birch CM, O'Neill NP, Hedequist DJ. Halo-gravity traction for the treatment of pediatric cervical spine disorders. J
Neurosurg Pediatr. 2019 Dec 27:1-10. doi: 10.3171/2019.10.PEDS19513. Epub ahead of print. PMID: 31881541.](https://image.slidesharecdn.com/cervicaltraction-230112173214-d5c6d549/85/Cervical-Traction-pptx-30-320.jpg)





