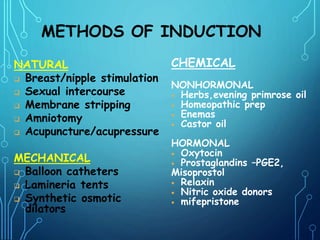
Induction of labor is the artificial initiation of uterine contractions before spontaneous labor, primarily during the third trimester, to facilitate a successful vaginal delivery. Indications for induction include maternal and fetal health threats, such as postterm pregnancy and medical conditions affecting the mother or fetus. Various methods exist for induction, including natural, mechanical, and chemical approaches, but certain contraindications and potential complications must be carefully assessed beforehand.