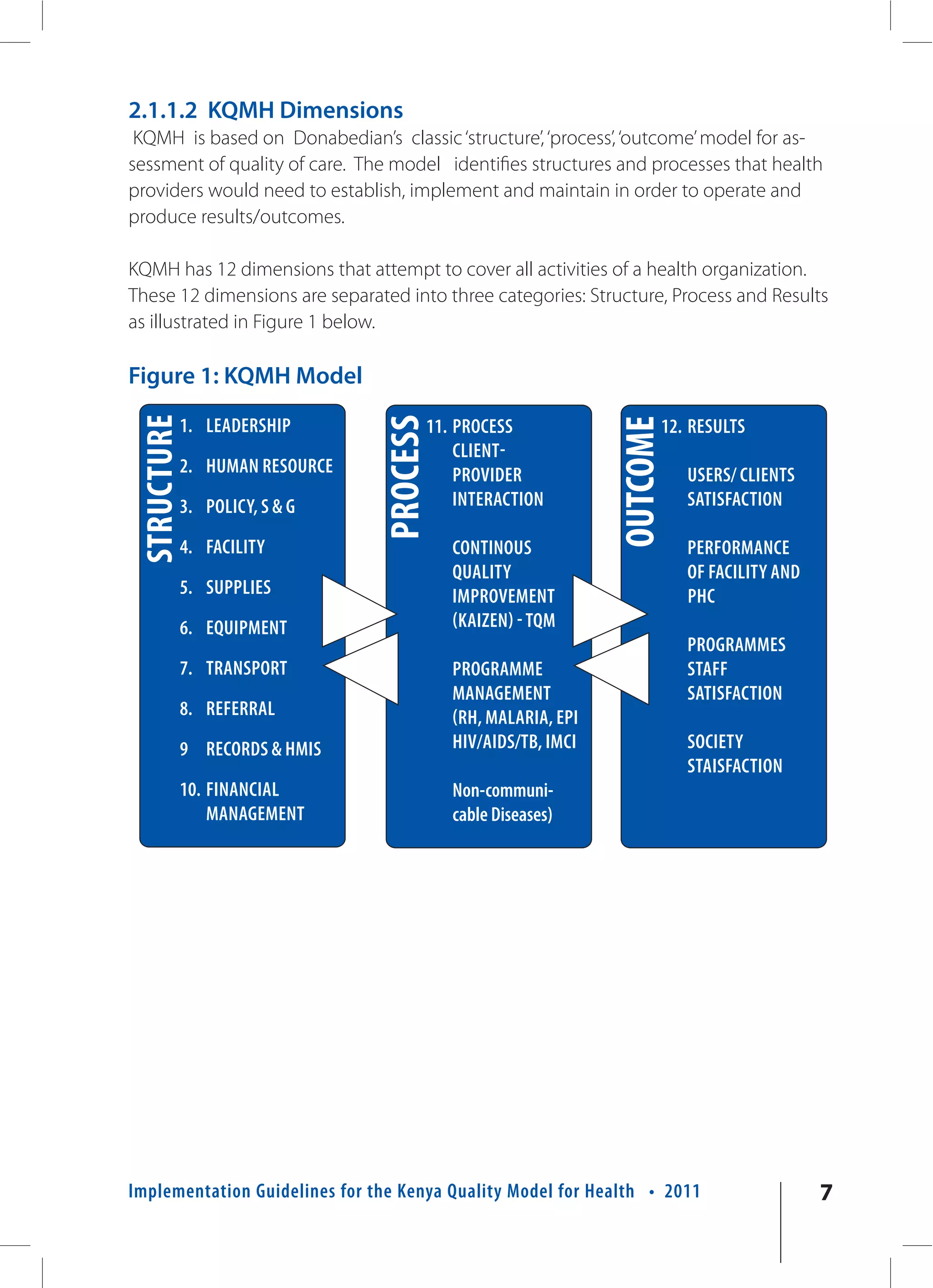
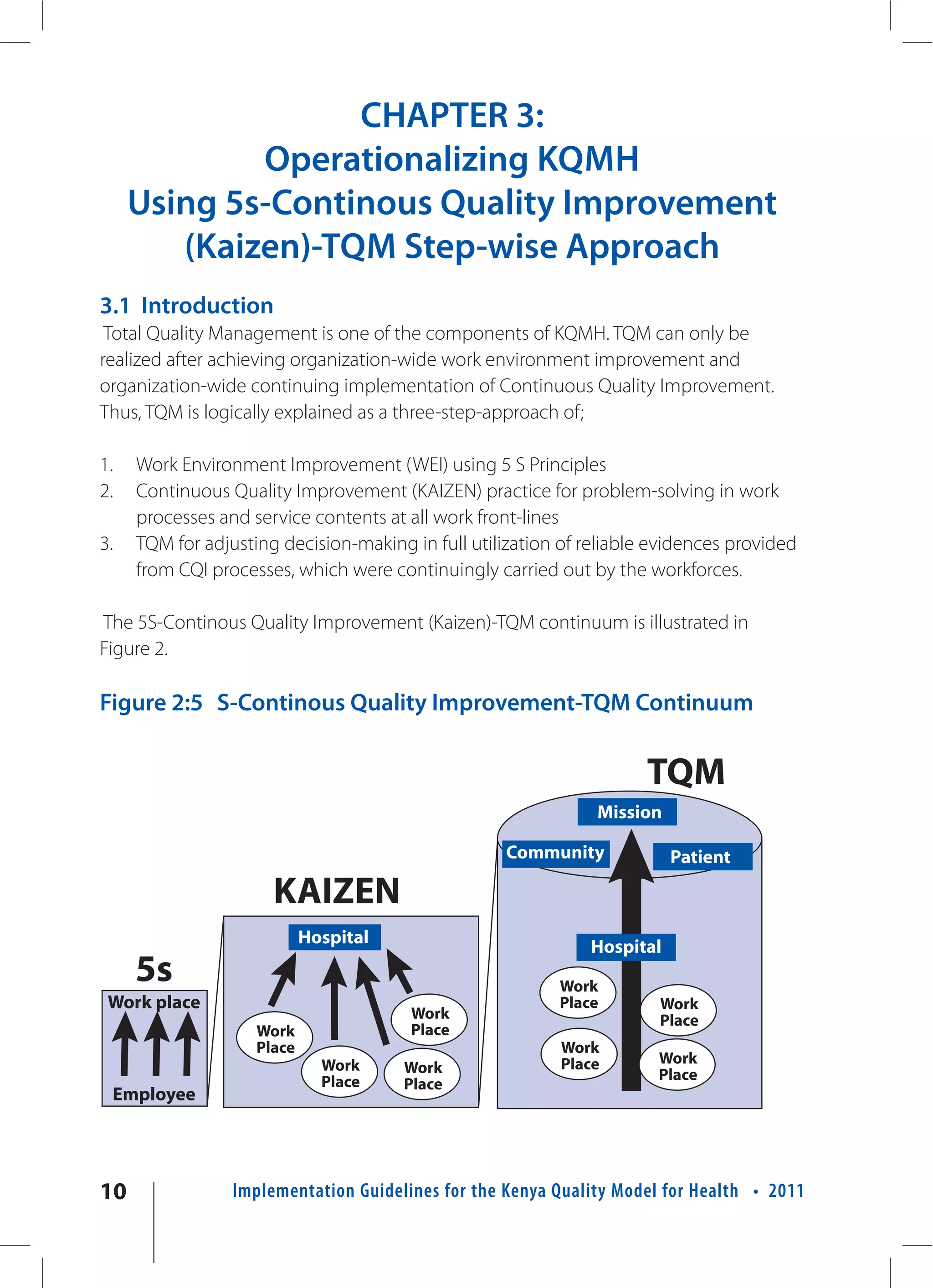
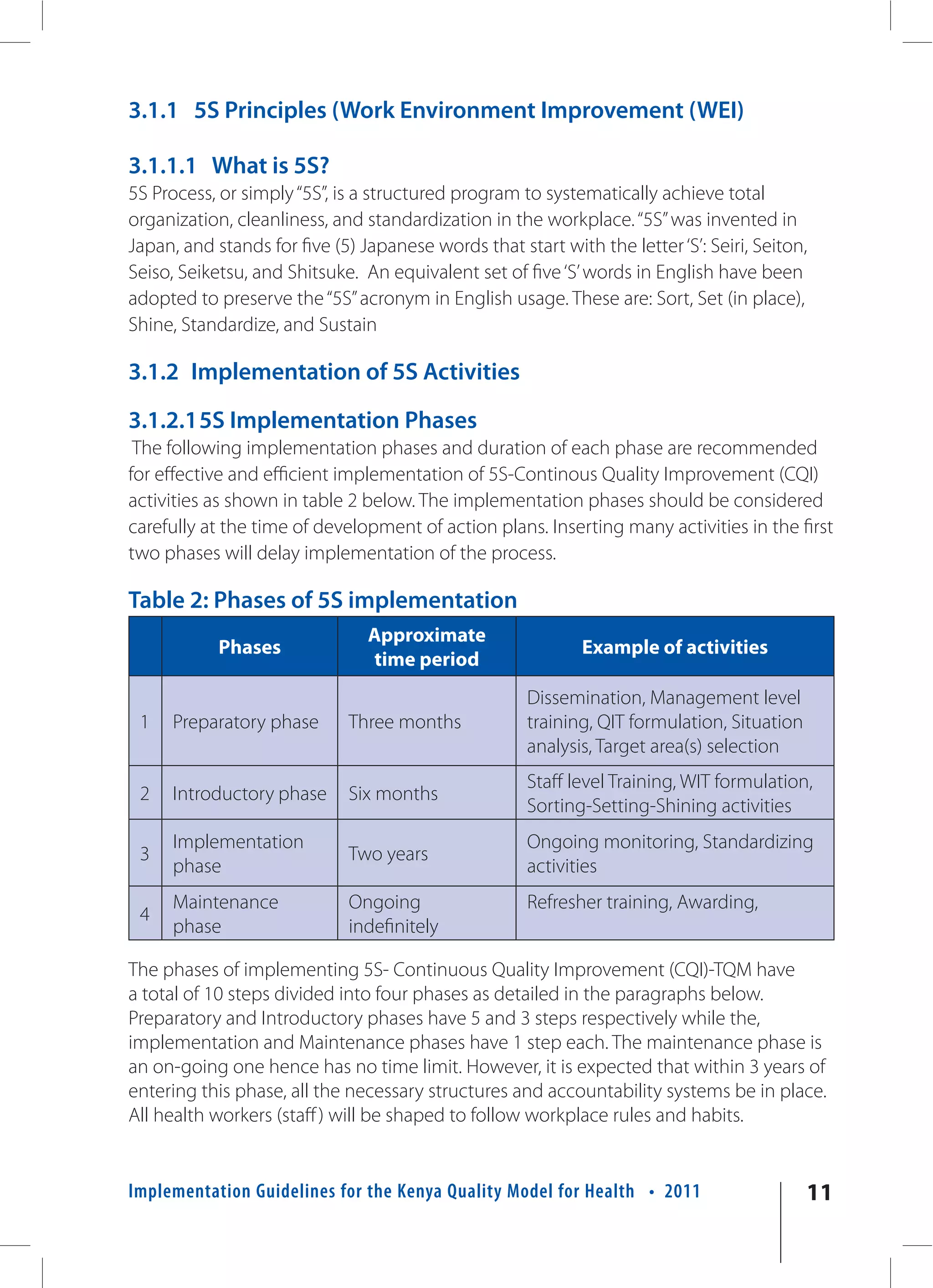
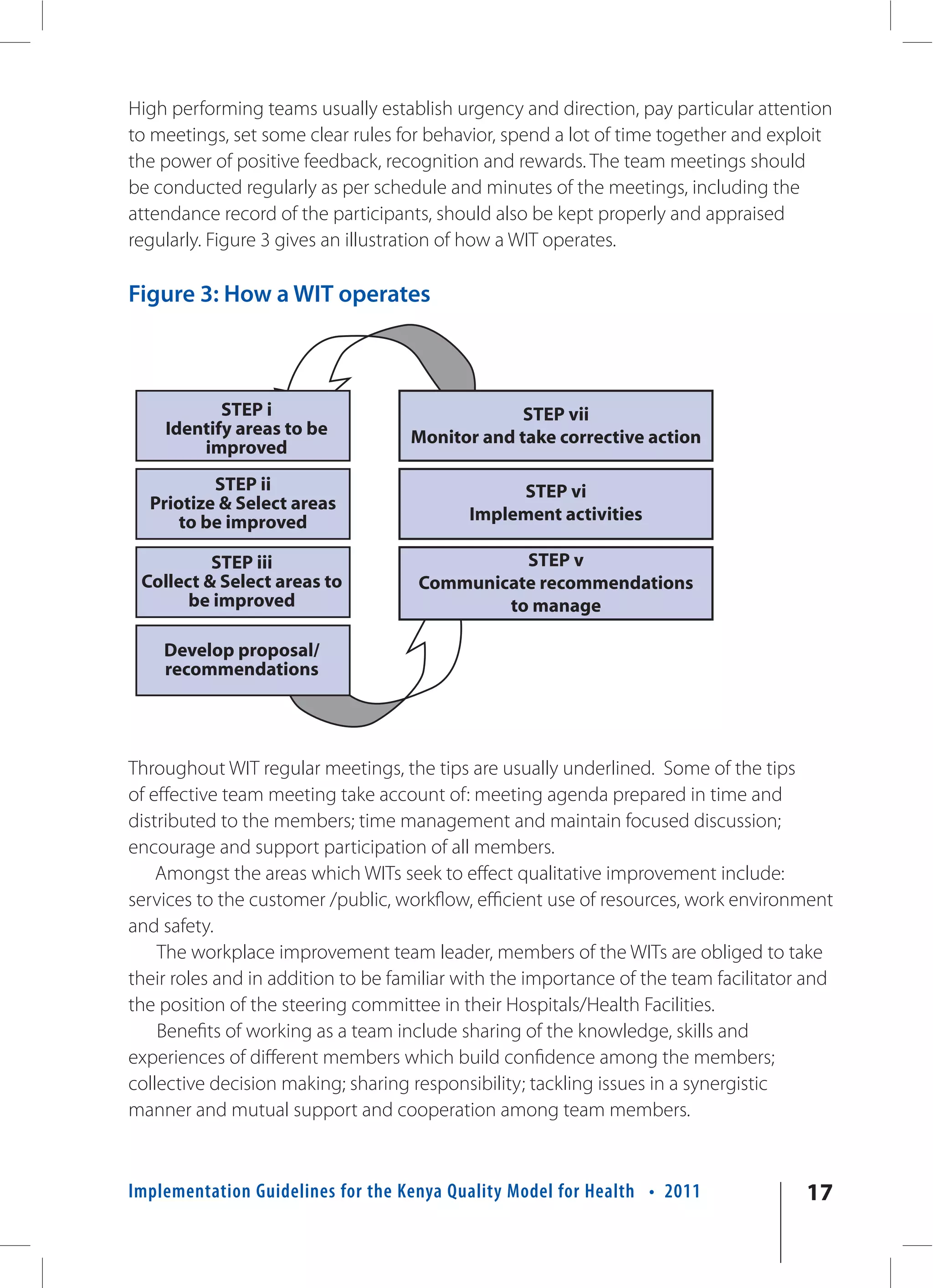
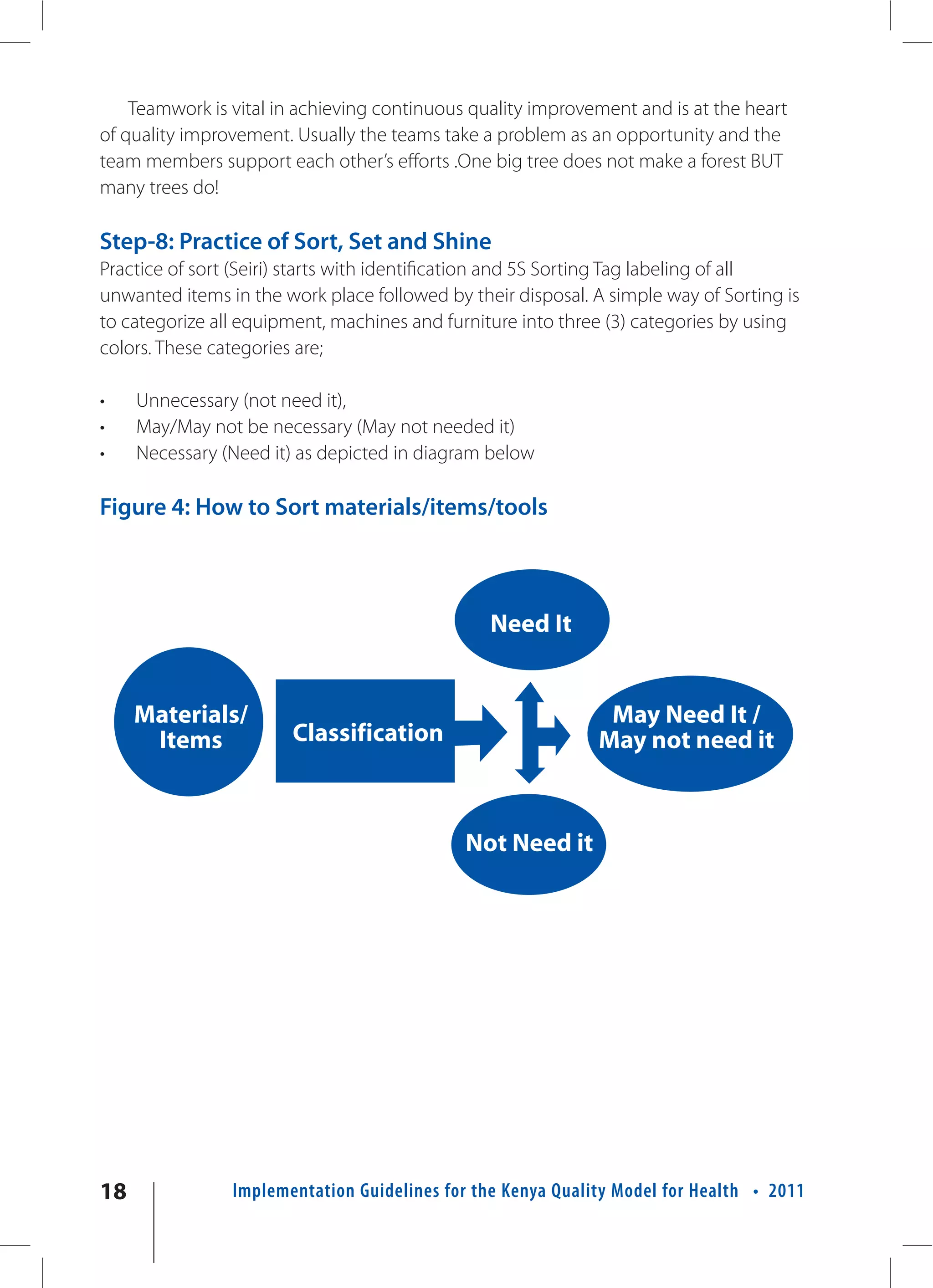
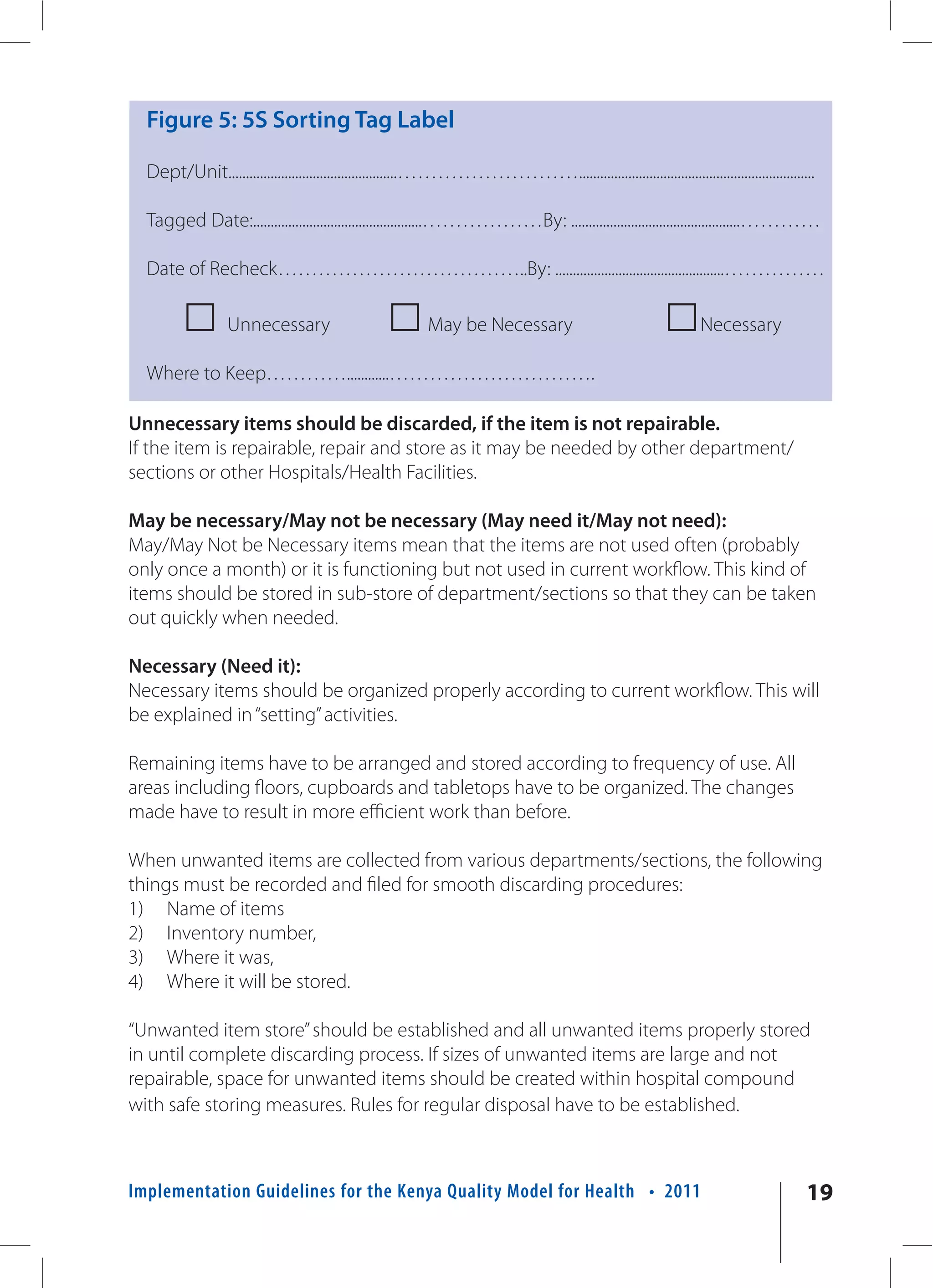
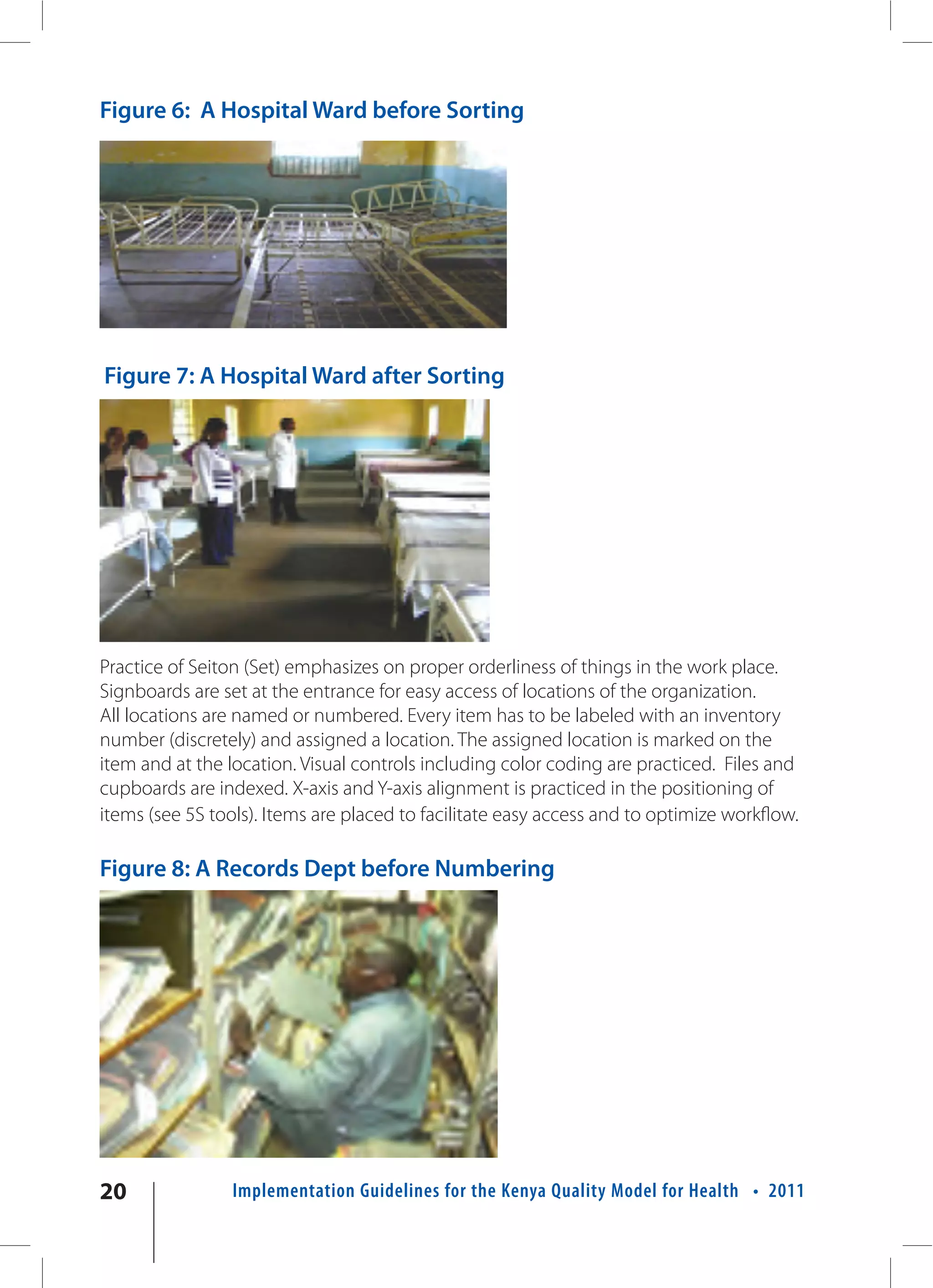
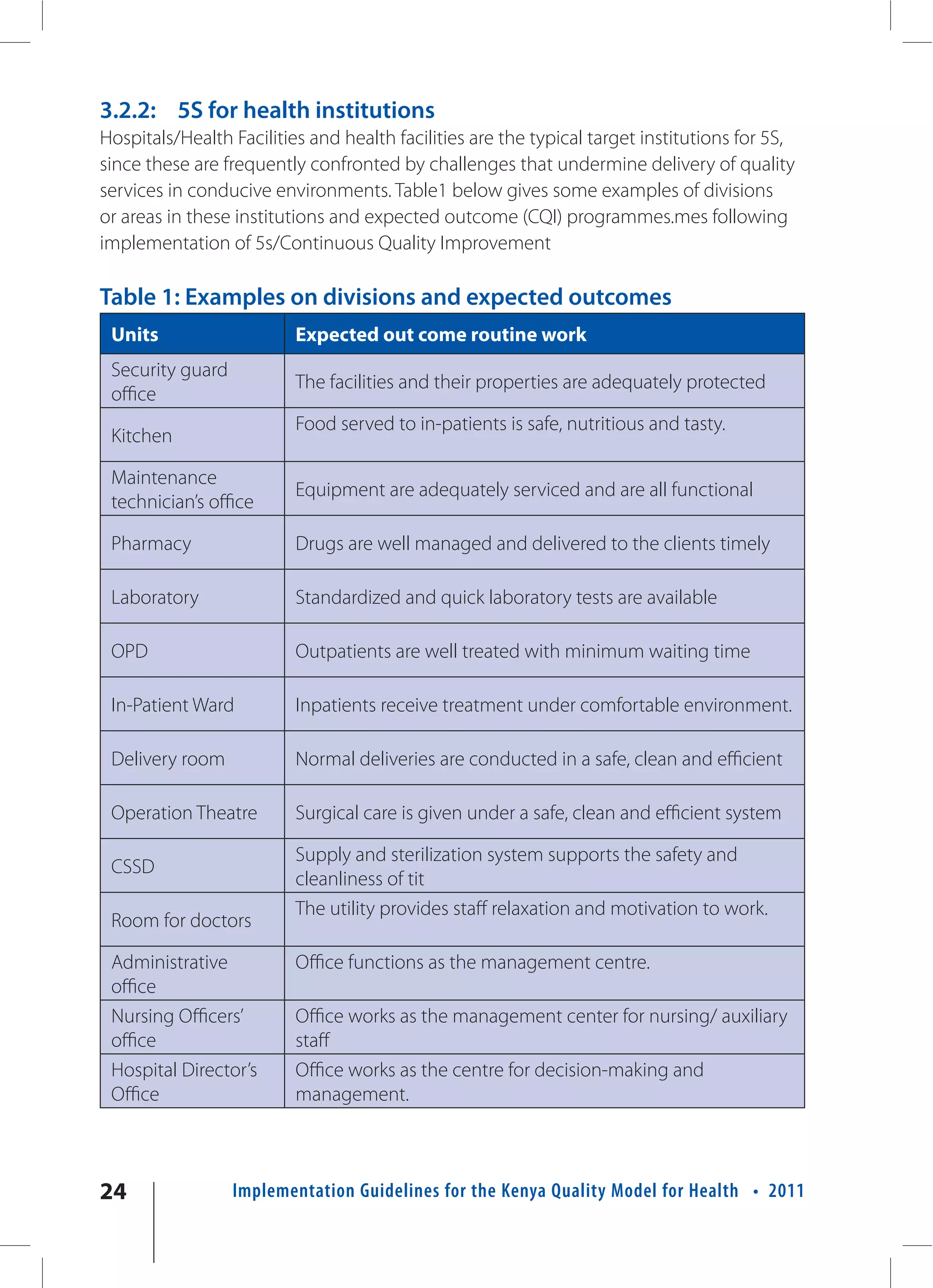
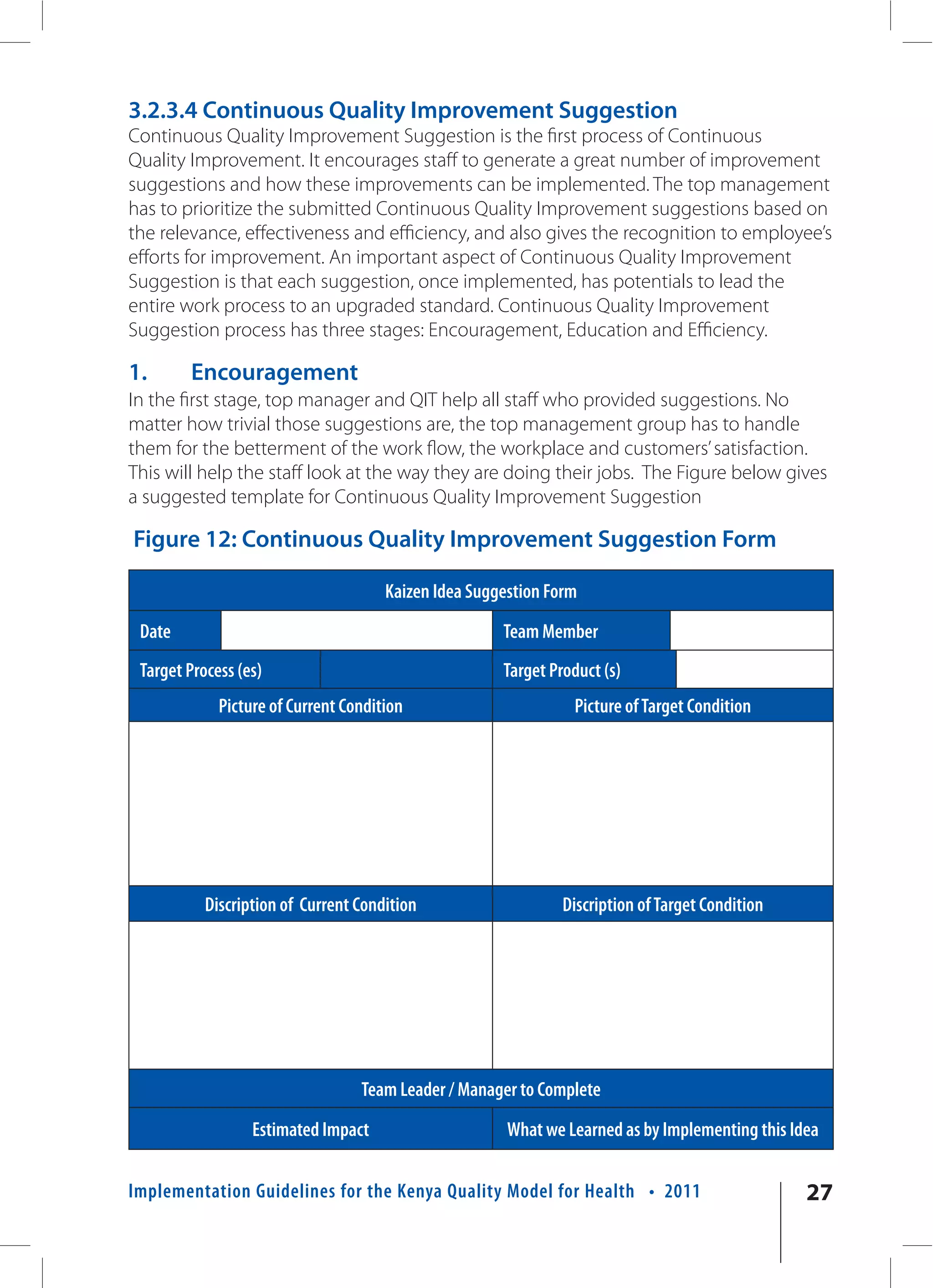
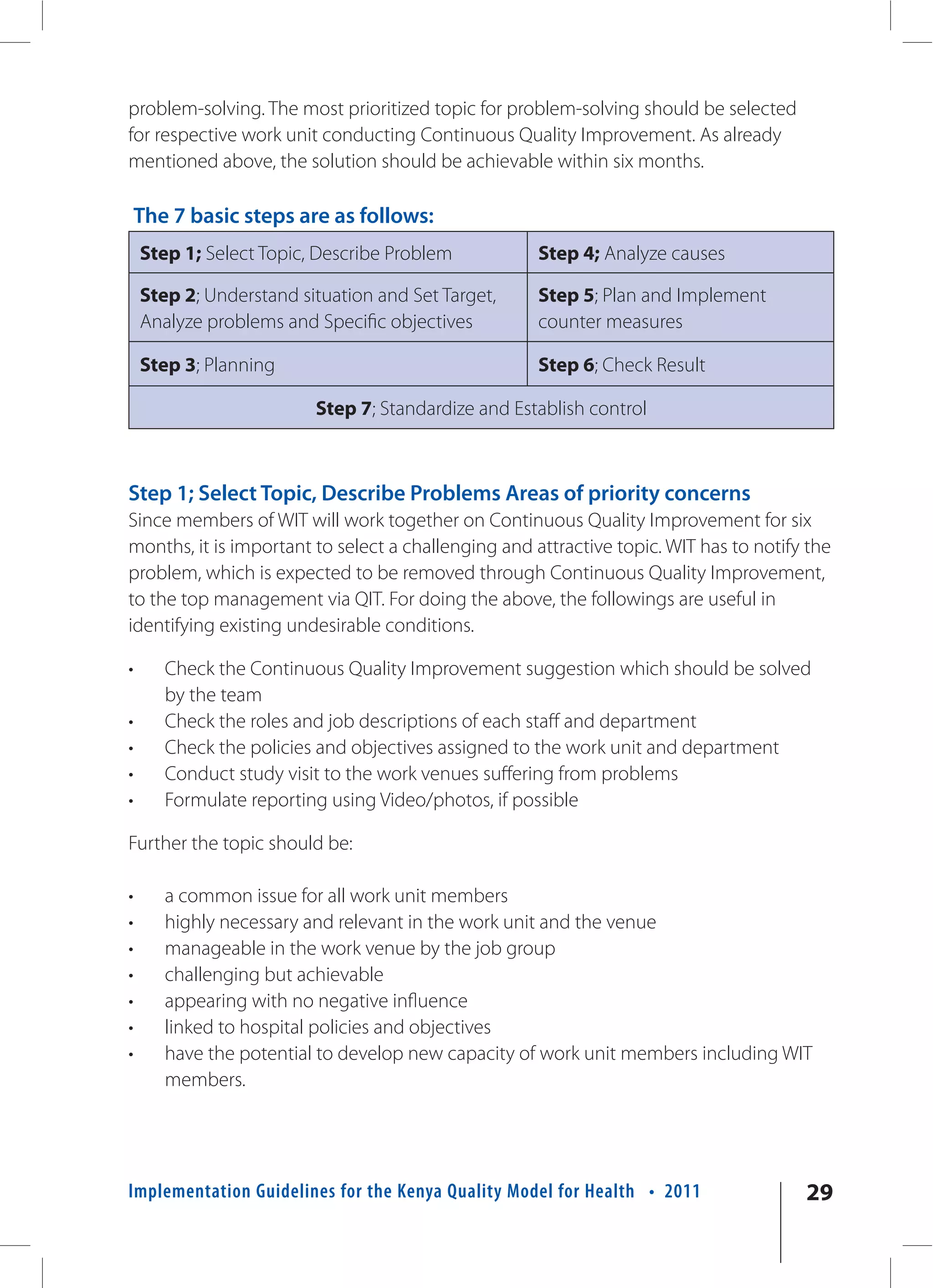
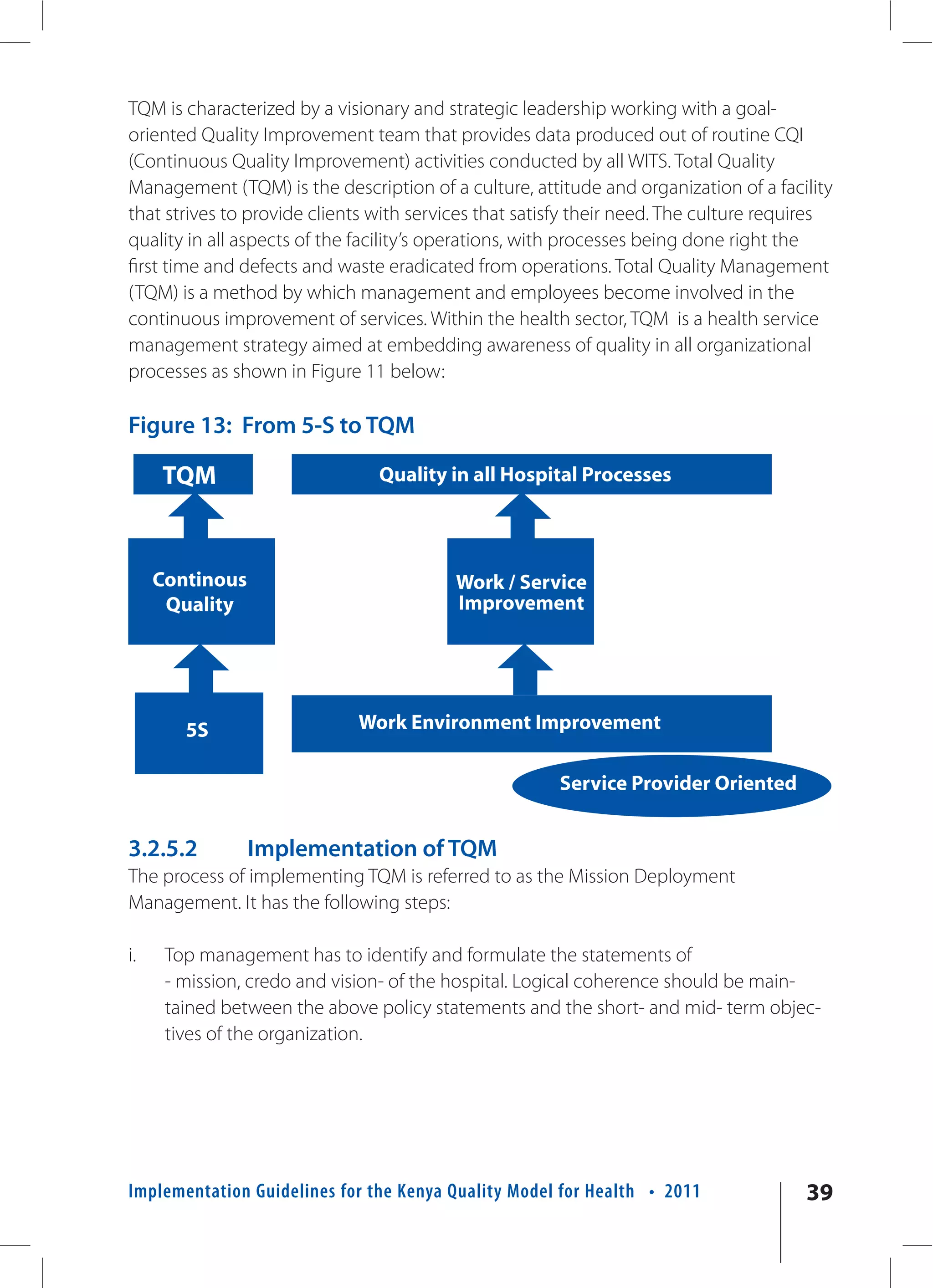
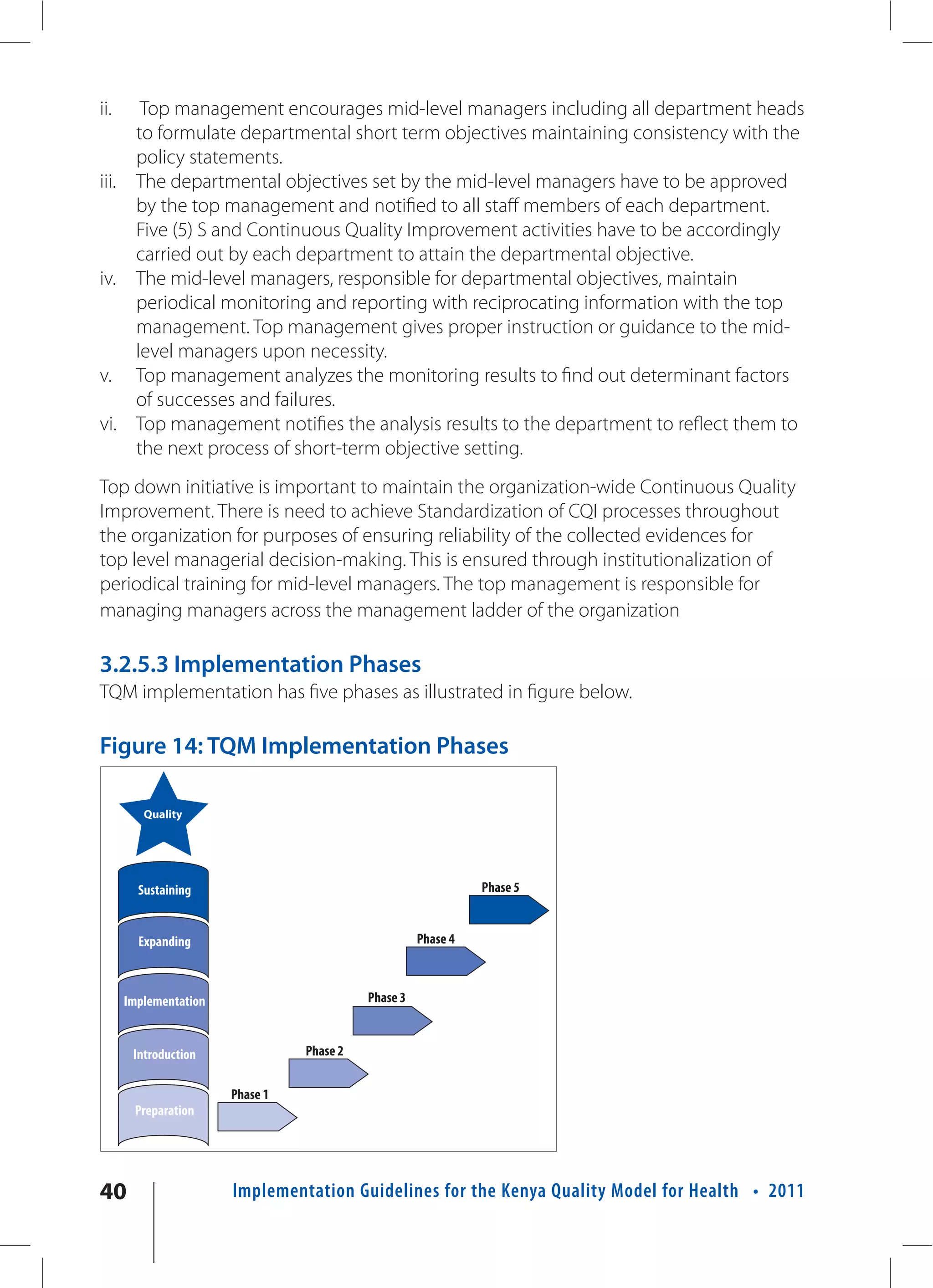
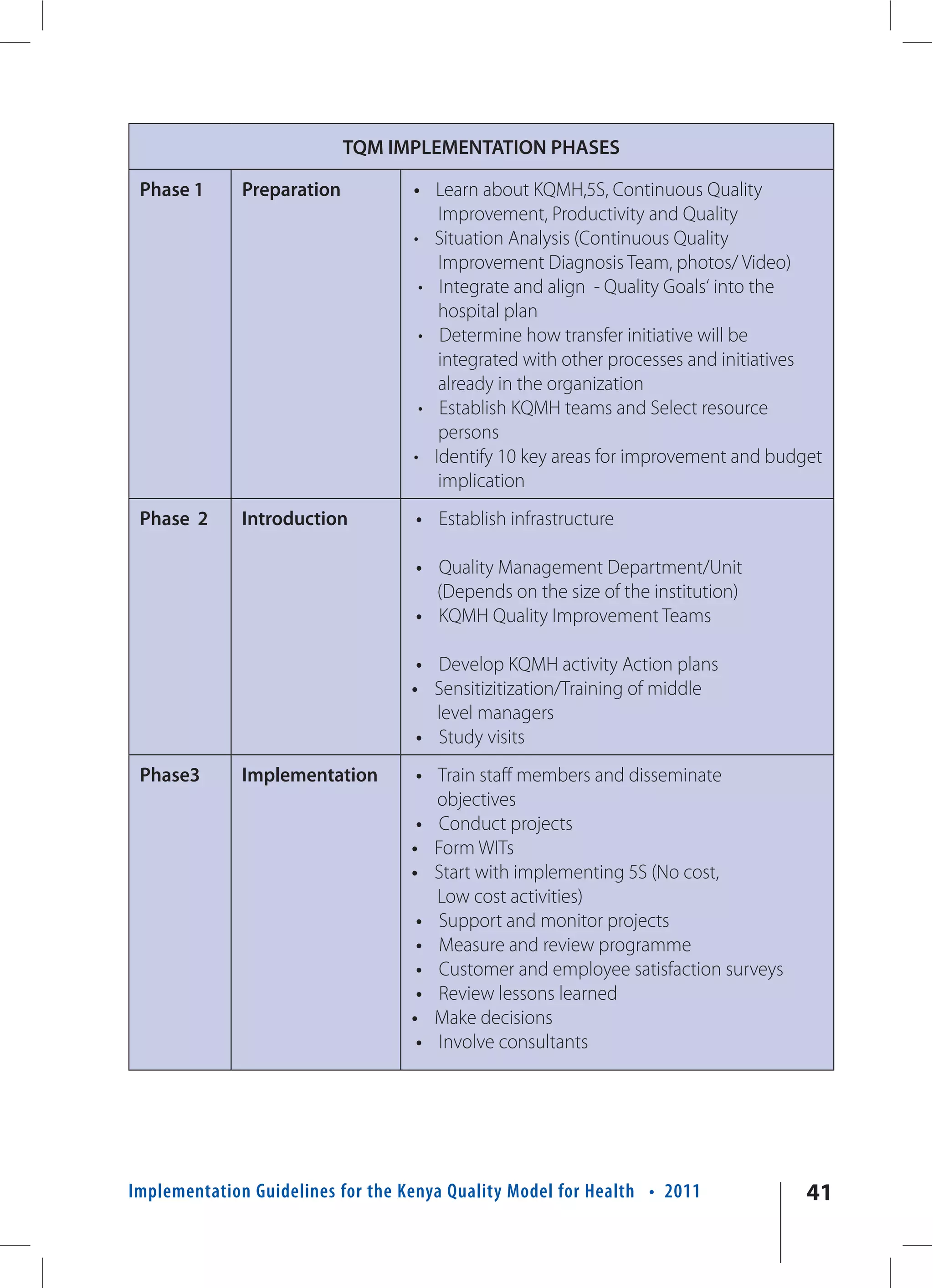
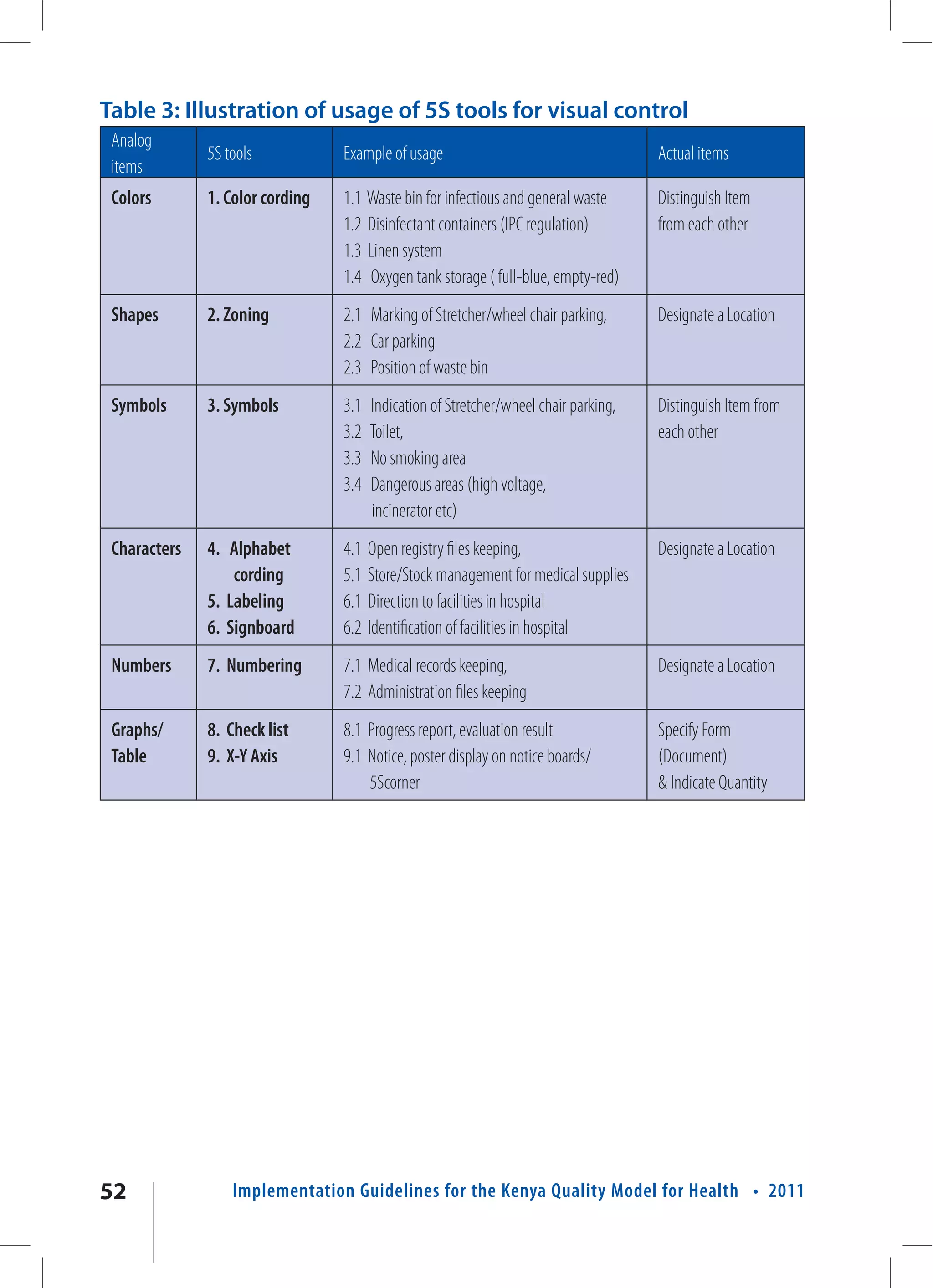
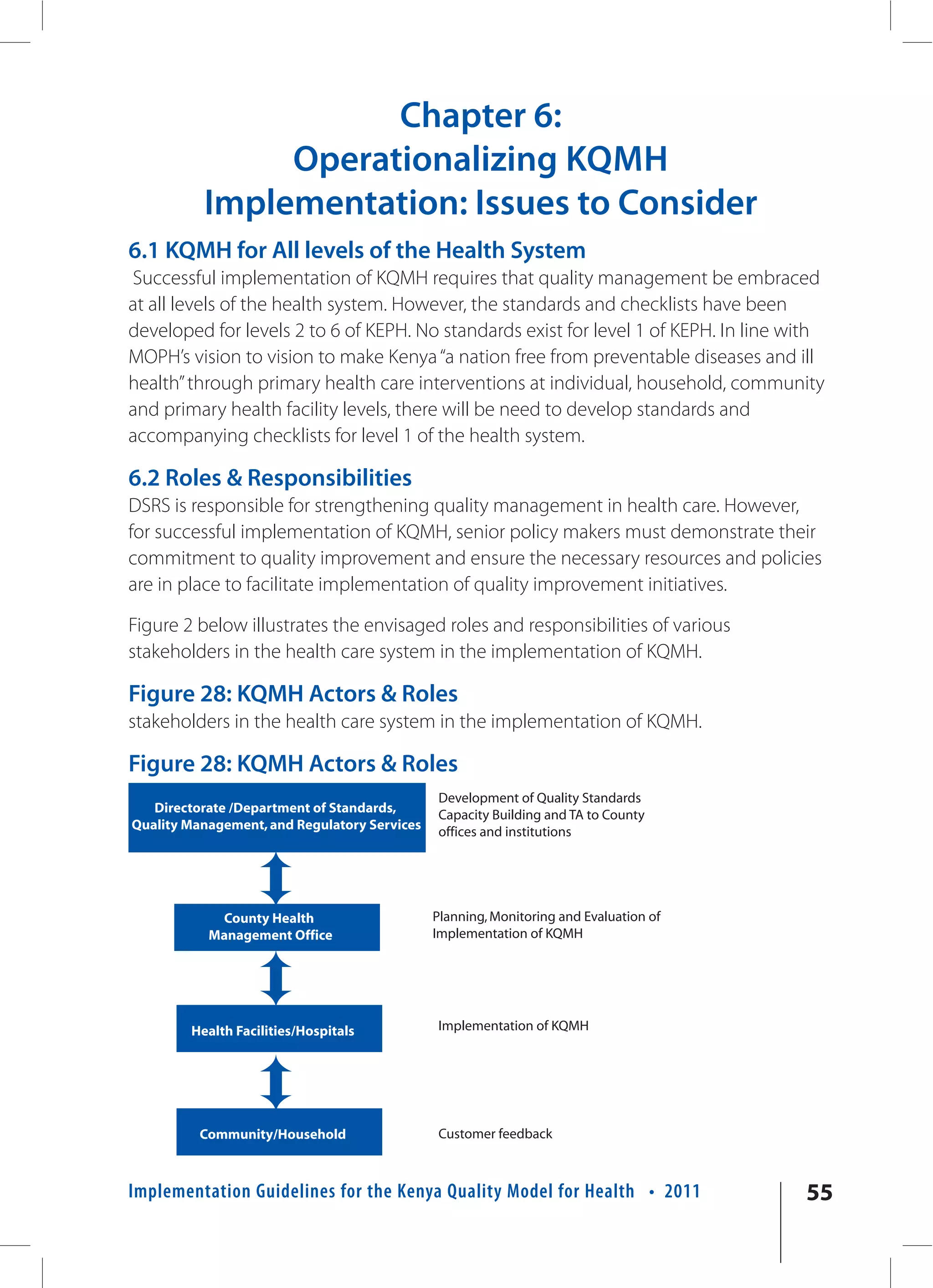
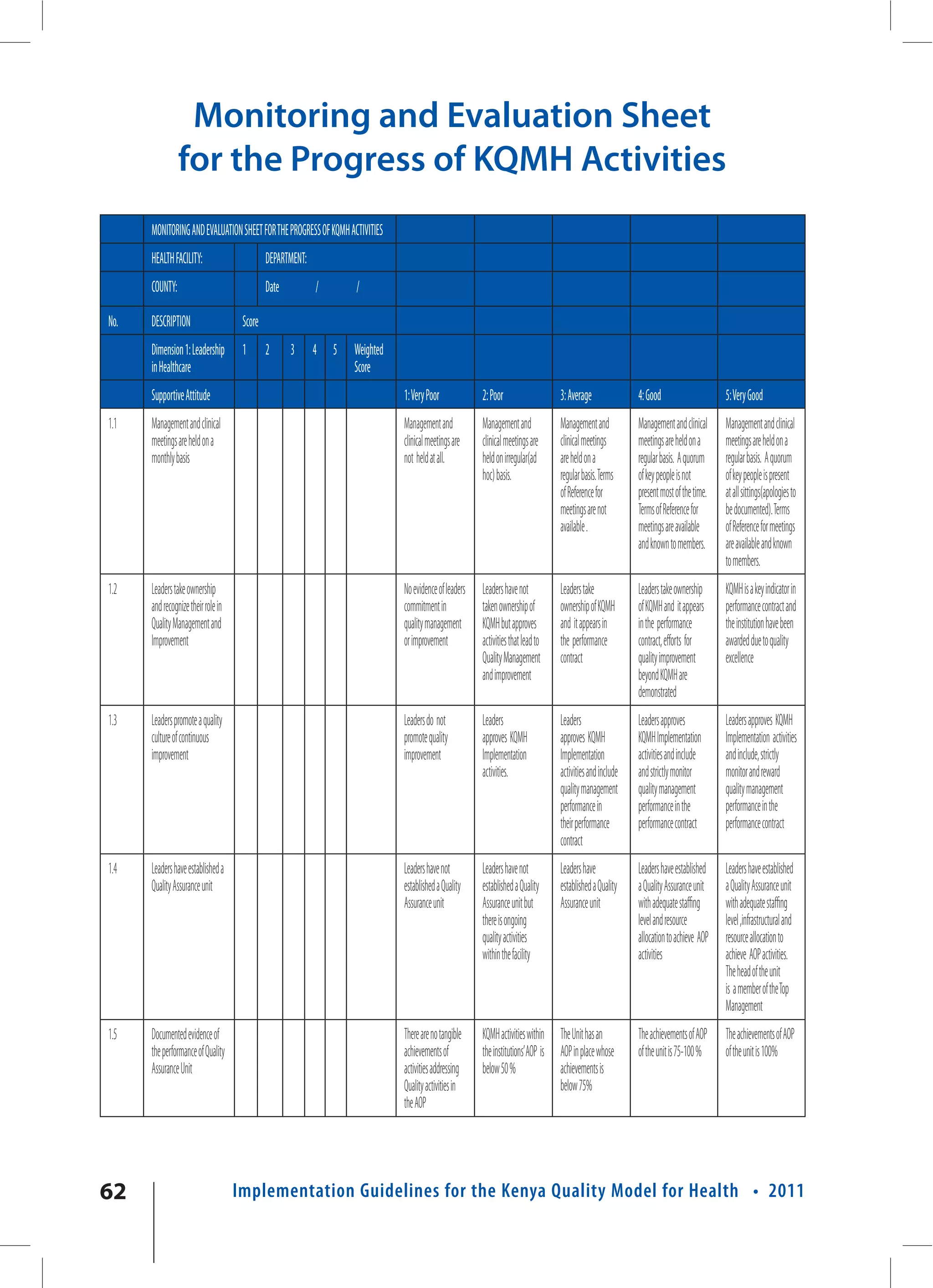
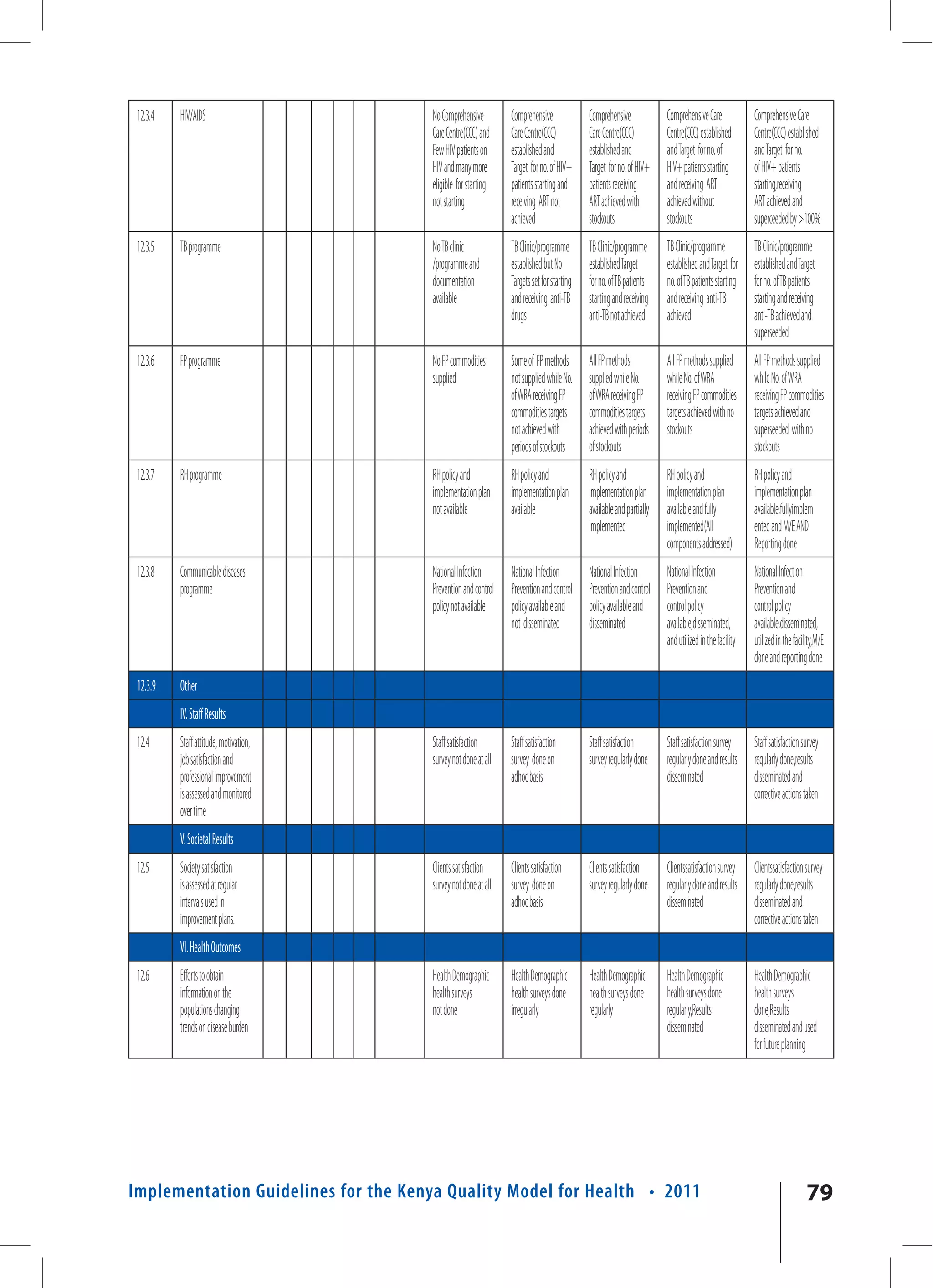
This document provides an overview of quality improvement initiatives in the Kenyan health sector. It discusses the Kenya Quality Model (KQM) and the Kenya Quality Model for Health (KQMH), which use a systems approach to management. The document also describes how the 5S principles of continuous quality improvement (CQI) - sorting, systematic arrangement, shine, standardization, and sustainability - can be implemented using a step-wise Total Quality Management (TQM) approach. This allows organizations to operationalize the KQMH. Various 5S and CQI tools are also outlined that can aid in the implementation of quality improvement activities according to the KQMH framework.