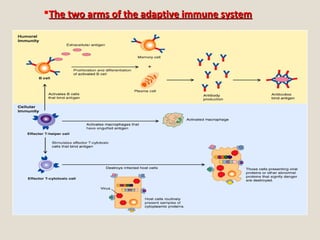
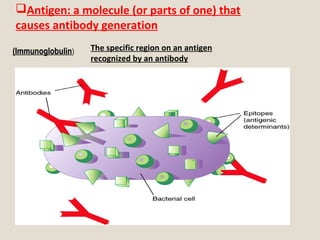
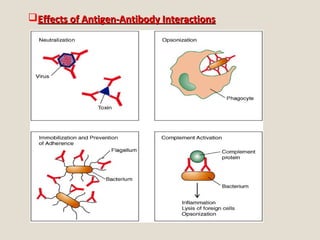
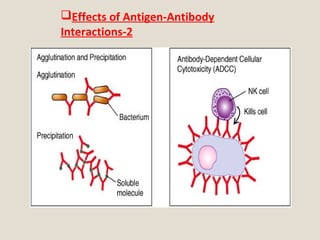
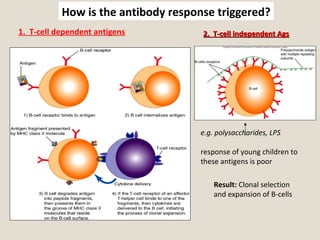
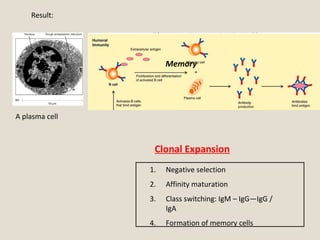
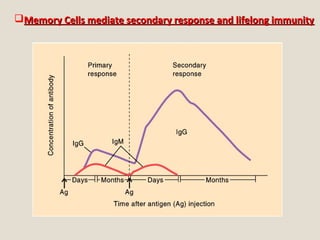
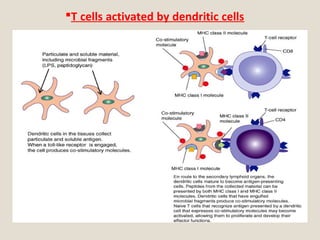
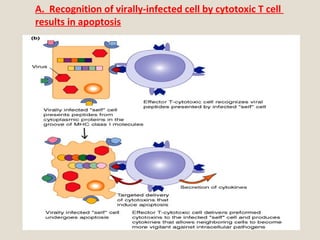
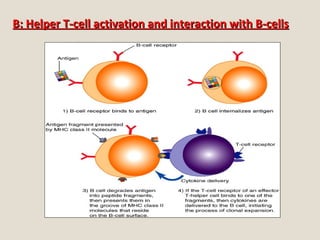
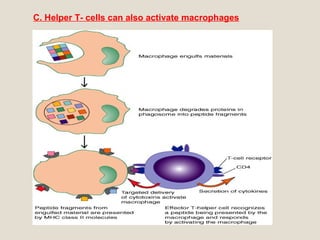
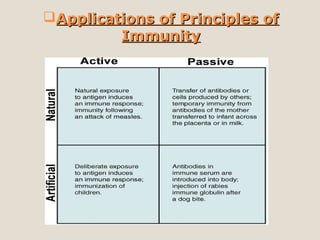
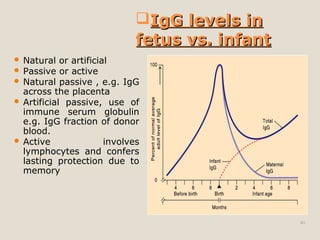
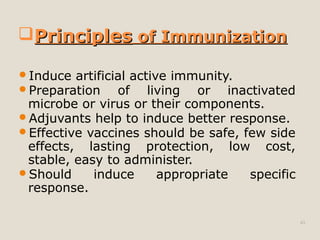
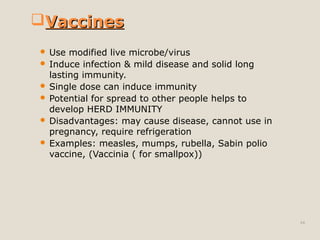
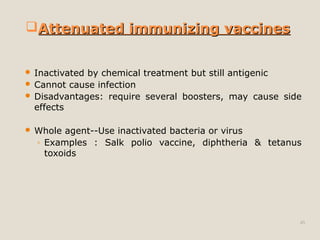
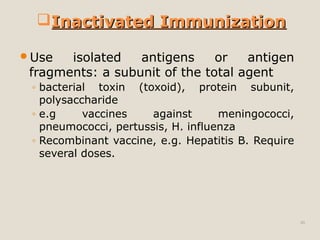
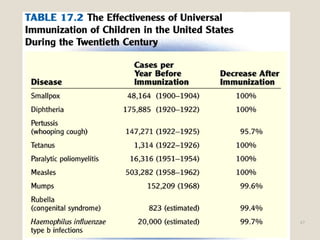
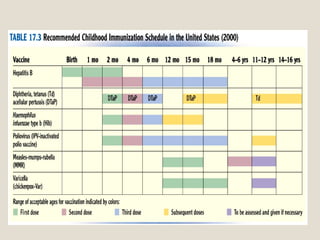
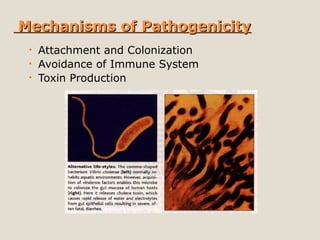
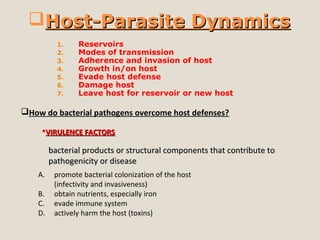
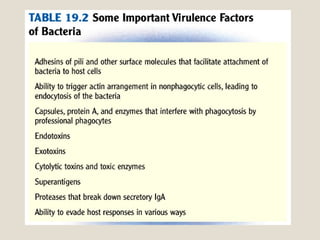
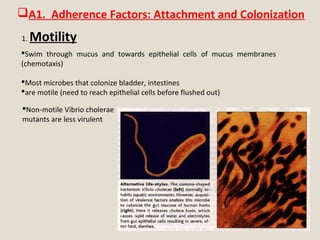
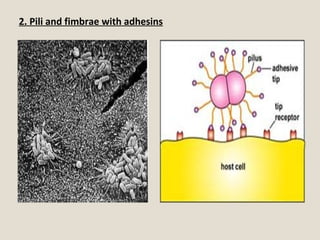
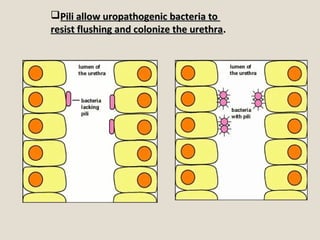
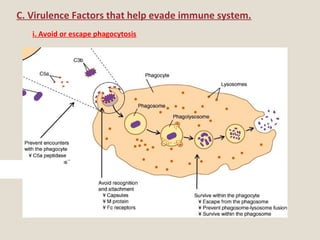
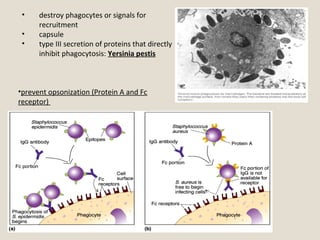
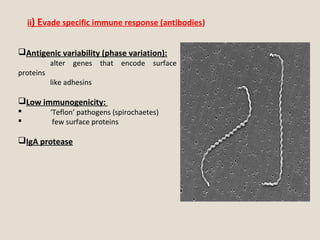
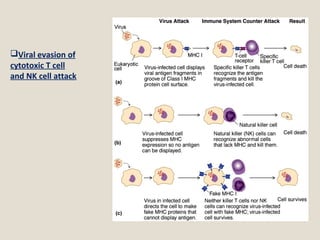
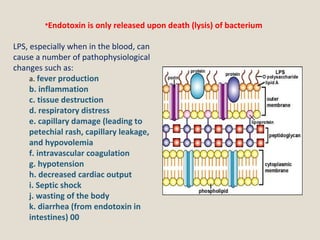
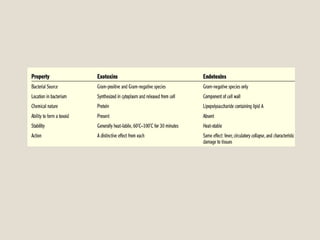
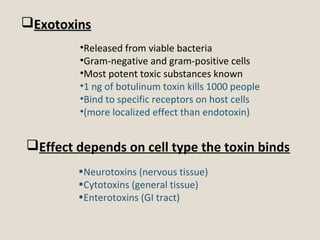
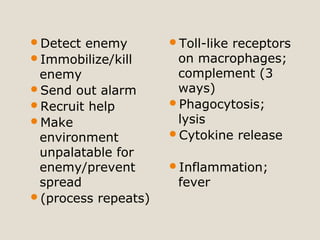
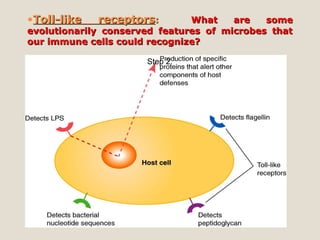
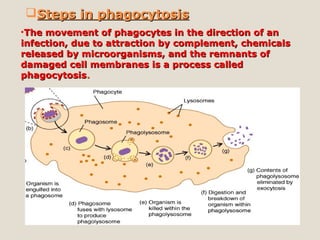
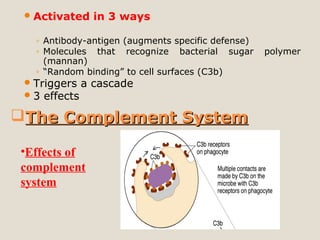
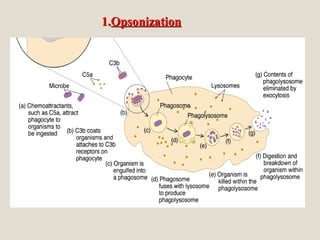
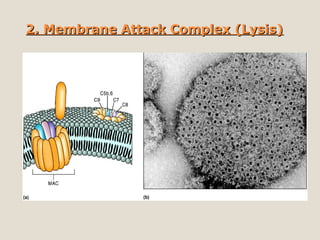
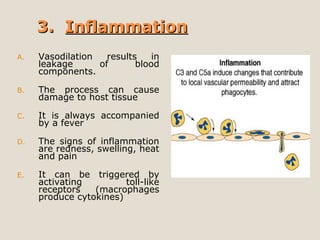
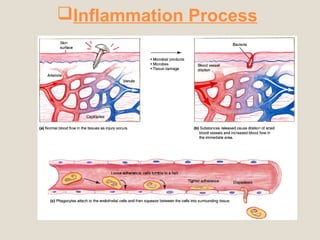
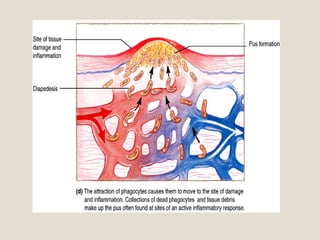
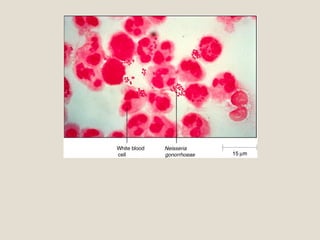
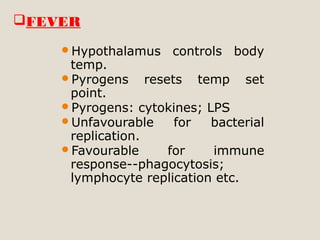
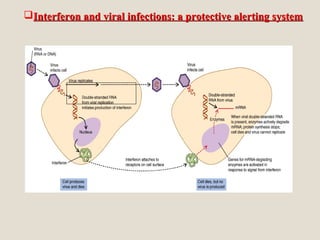
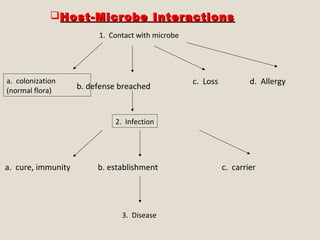
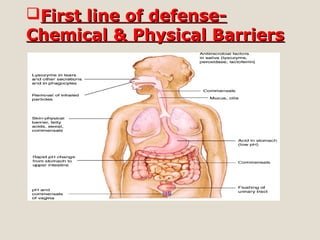
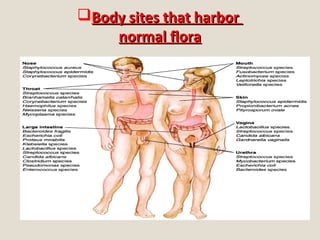
The document provides an overview of the immune system, detailing its three lines of defense: non-specific innate immunity (first and second lines) involving physical barriers, phagocytosis, inflammation, and fever, and specific adaptive immunity (third line) involving T and B cells along with antibodies. It discusses the importance of normal flora in preventing infections, the complement system's role in defense, and how various factors, including antigens and virulence factors, affect host-pathogen interactions. Additionally, it covers the mechanisms of immunization, vaccine types, and the genetic basis of pathogenicity.
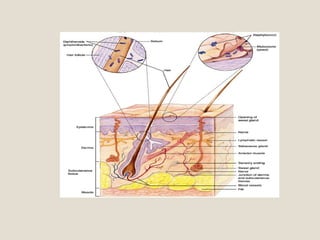
![Normal Skin FloraNormal Skin Flora
1000 to >1 million/ cm2
Diphtheroids: G+ rods & cocci, e.g.
Corynebacterium & Proprionobacterium ,
e.g. P.acnes (acne)
facultatively anaerobic, coagulase
negative Staphylococci [carriers of
coagulase positive S. aureus in
population]
Yeasts](https://image.slidesharecdn.com/14-181130150810/85/Immunology-and-Microbiology-Host-Microbe-Interactions-23-320.jpg)