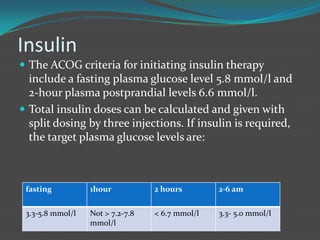
Gestational diabetes is a form of diabetes that develops during pregnancy and usually resolves after giving birth. It occurs when hormones produced during pregnancy interfere with the mother's body's ability to produce and use insulin properly. This can cause high blood glucose levels. Left untreated, gestational diabetes can increase the risk of complications for both mother and baby, such as preeclampsia in the mother, and macrosomia, shoulder dystocia, and jaundice in the baby. It is diagnosed through a glucose tolerance test between 24-28 weeks of gestation. Treatment may involve lifestyle modifications like diet and exercise or insulin therapy if needed. Close monitoring during pregnancy and screening for diabetes after pregnancy is important.