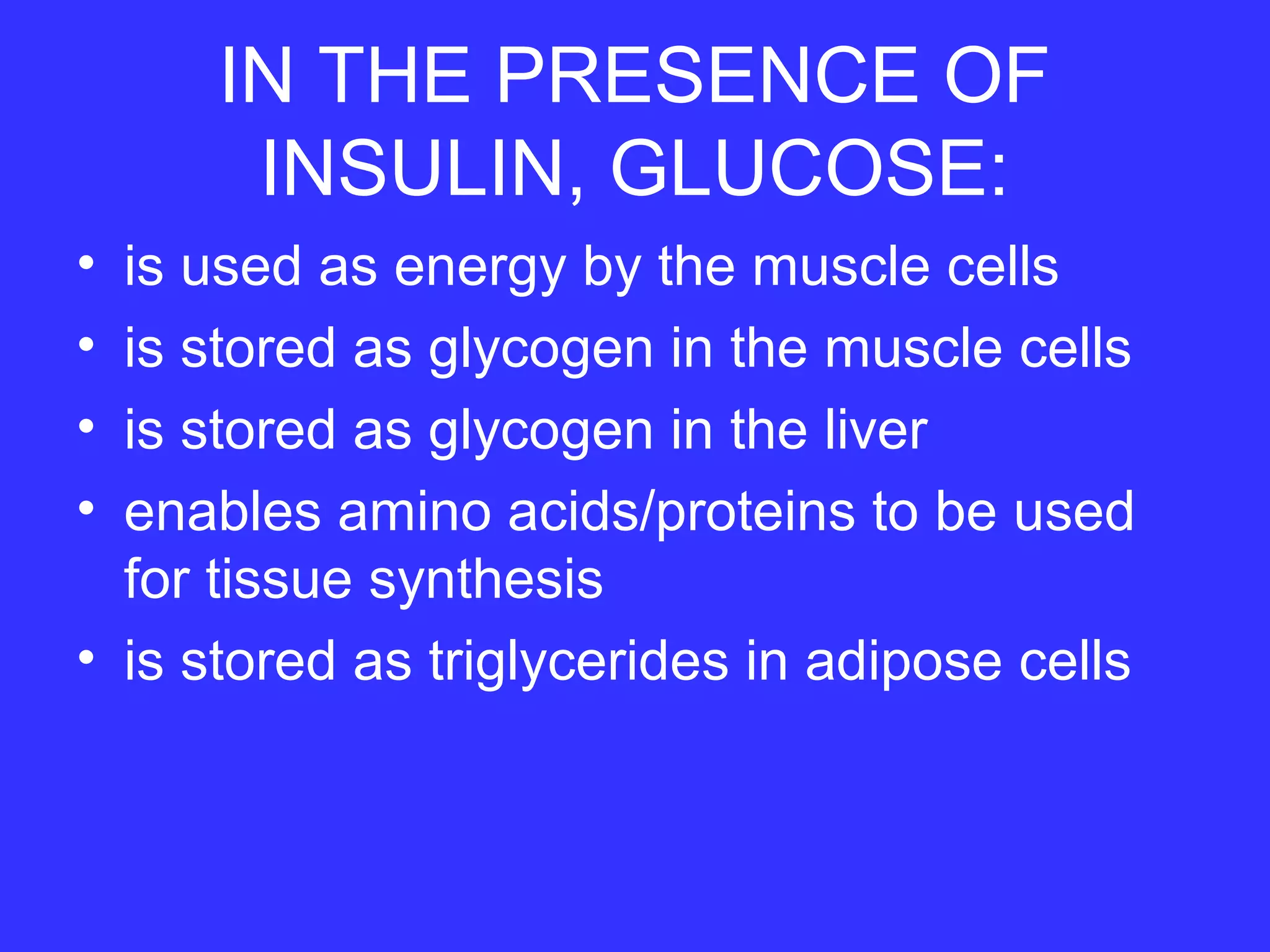
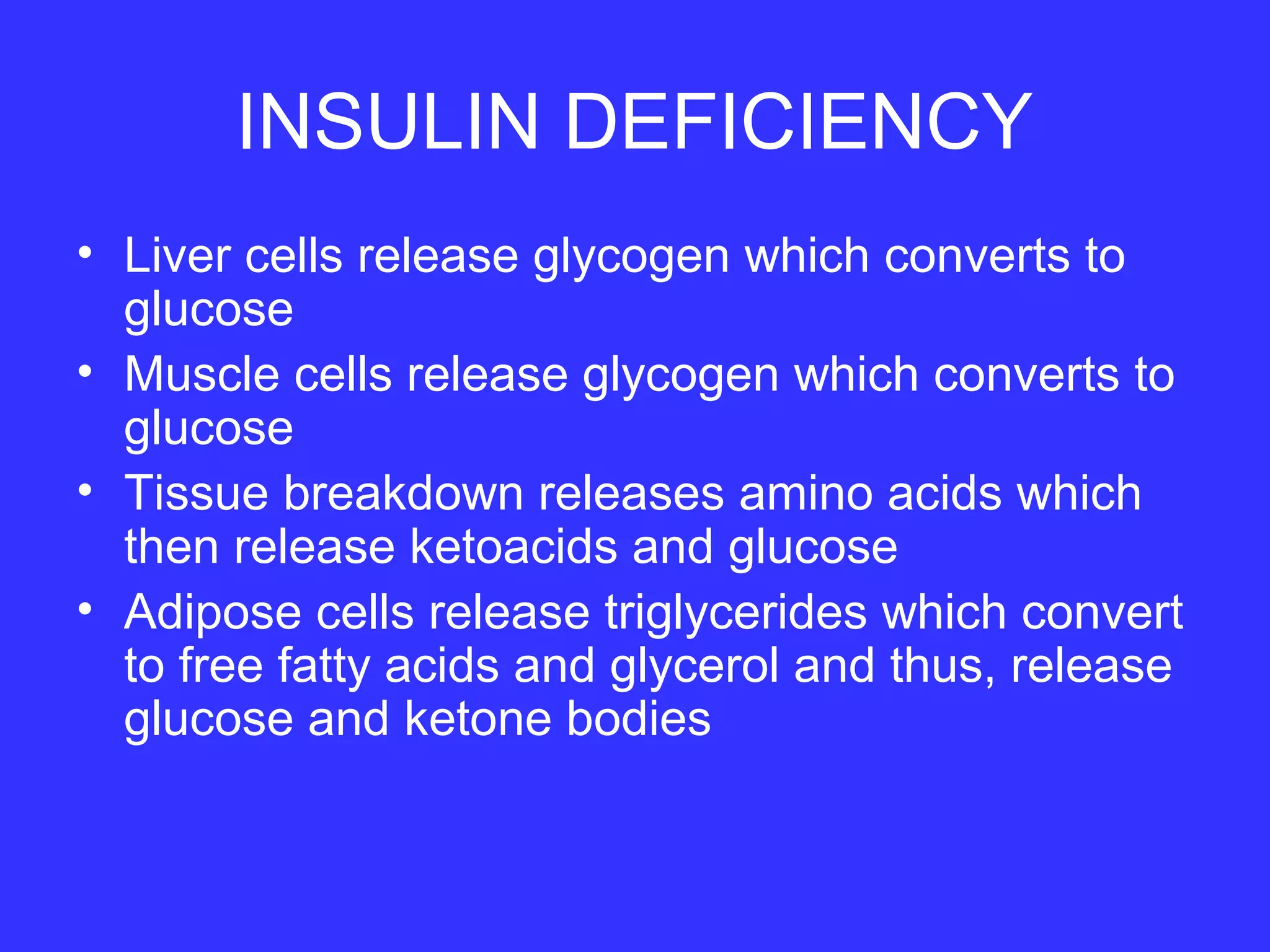
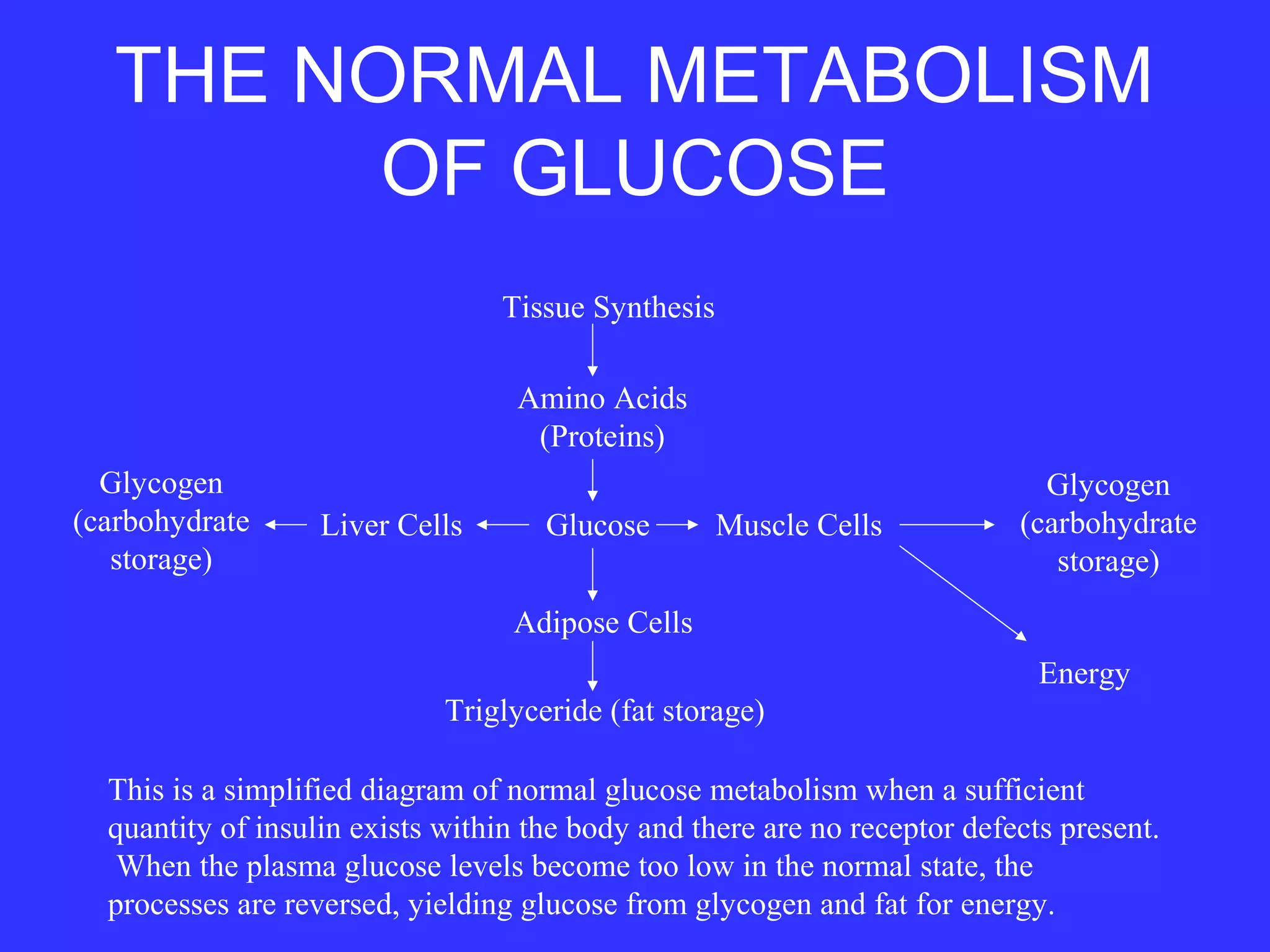
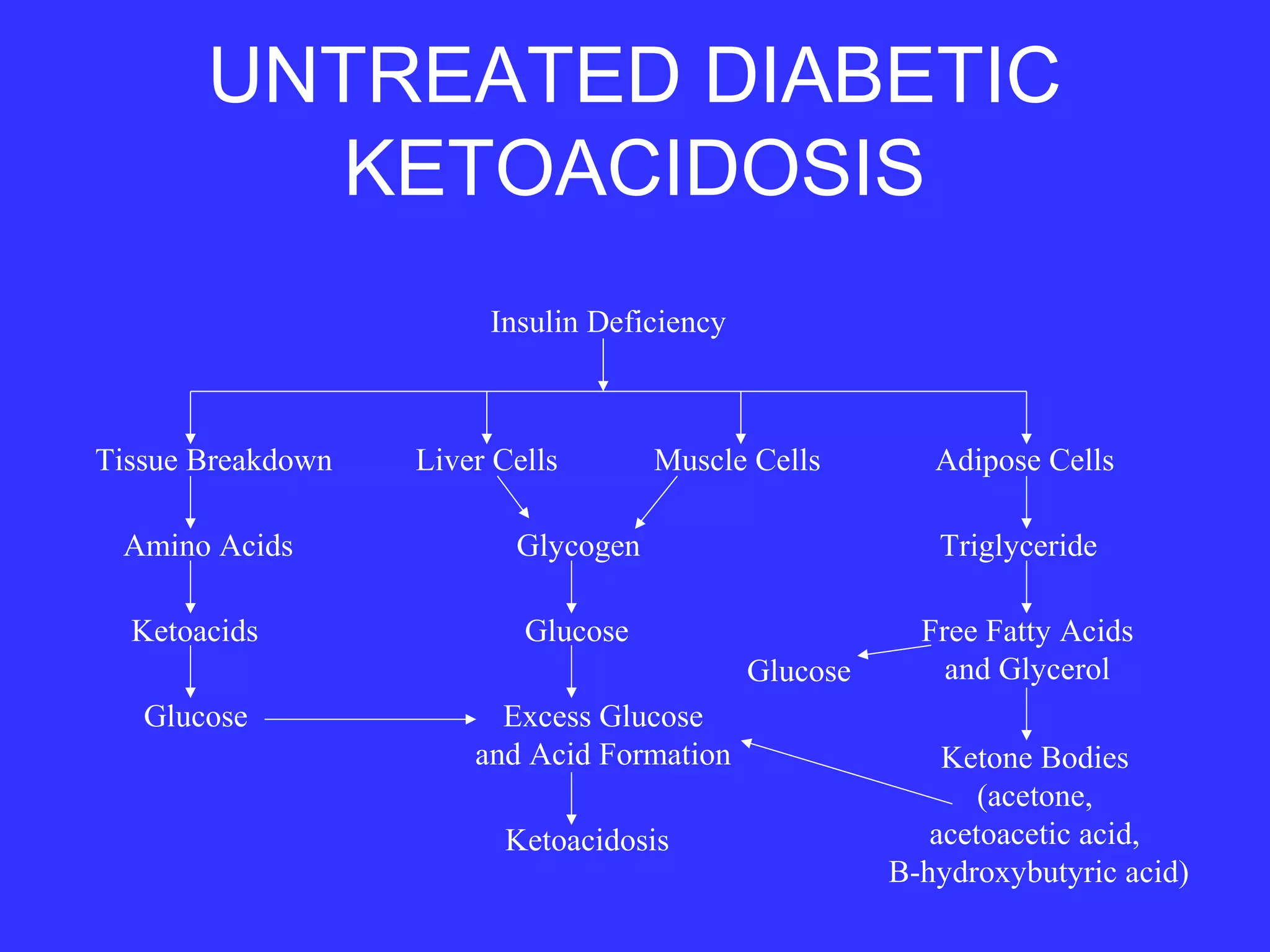
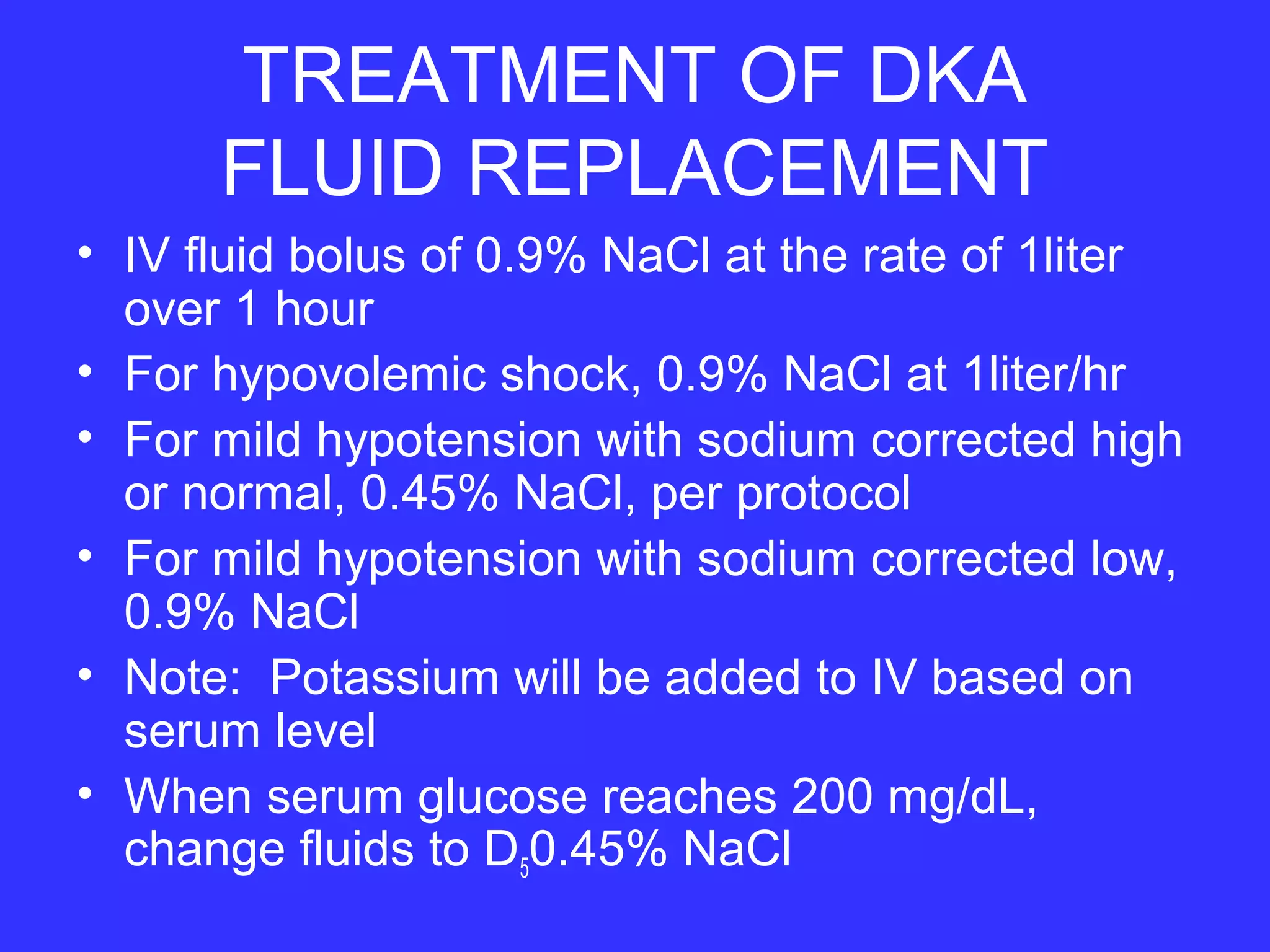
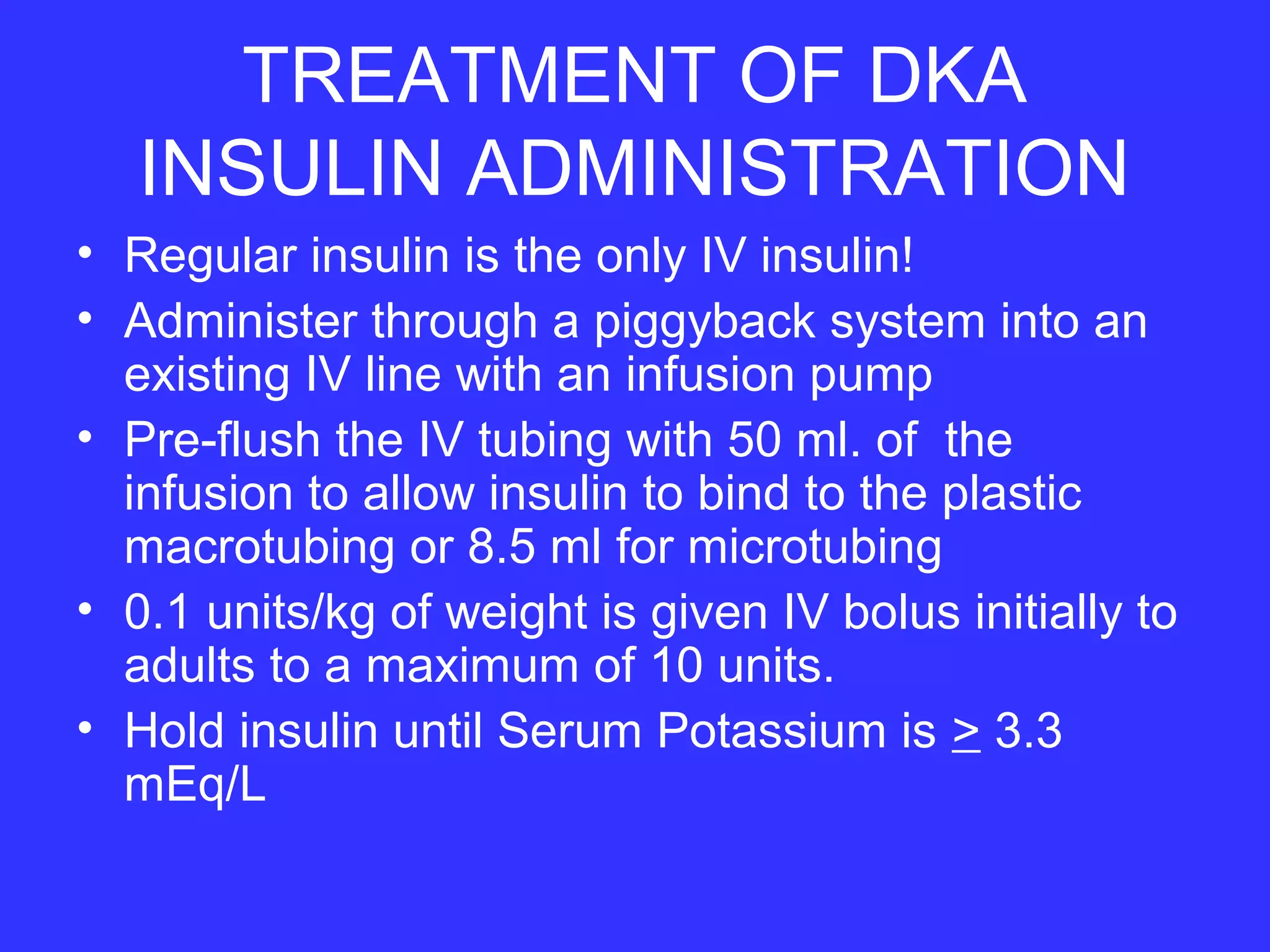
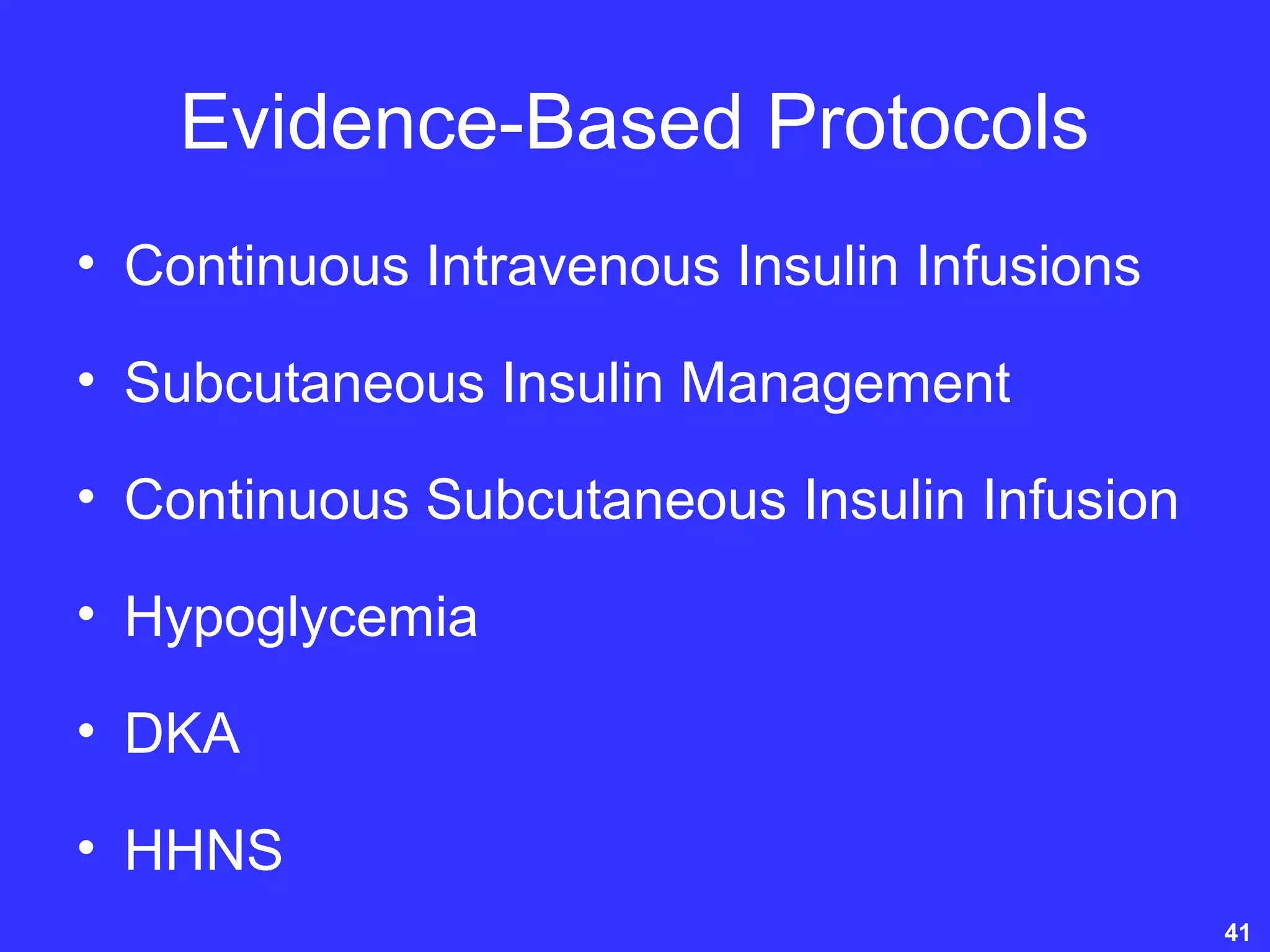
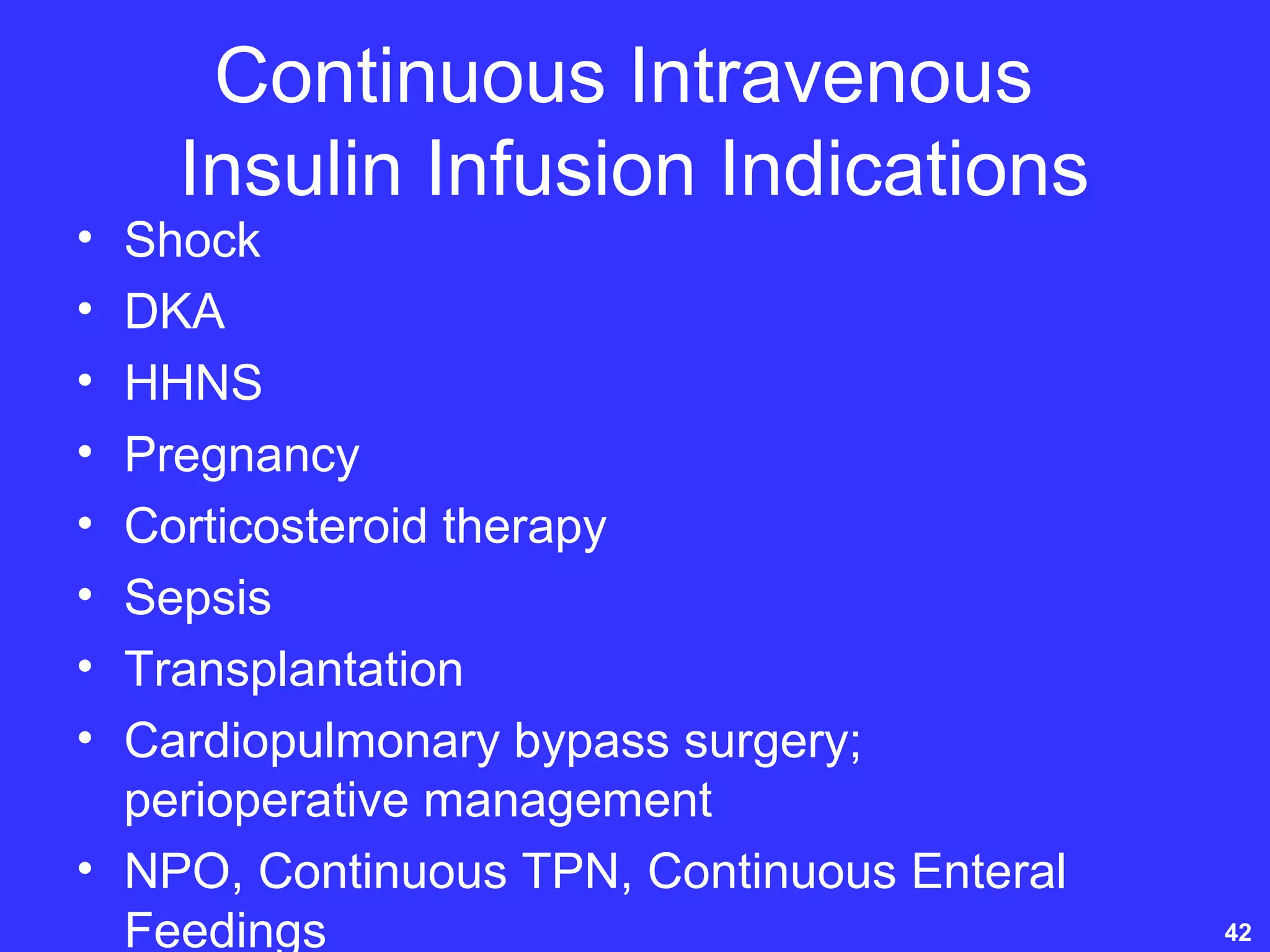
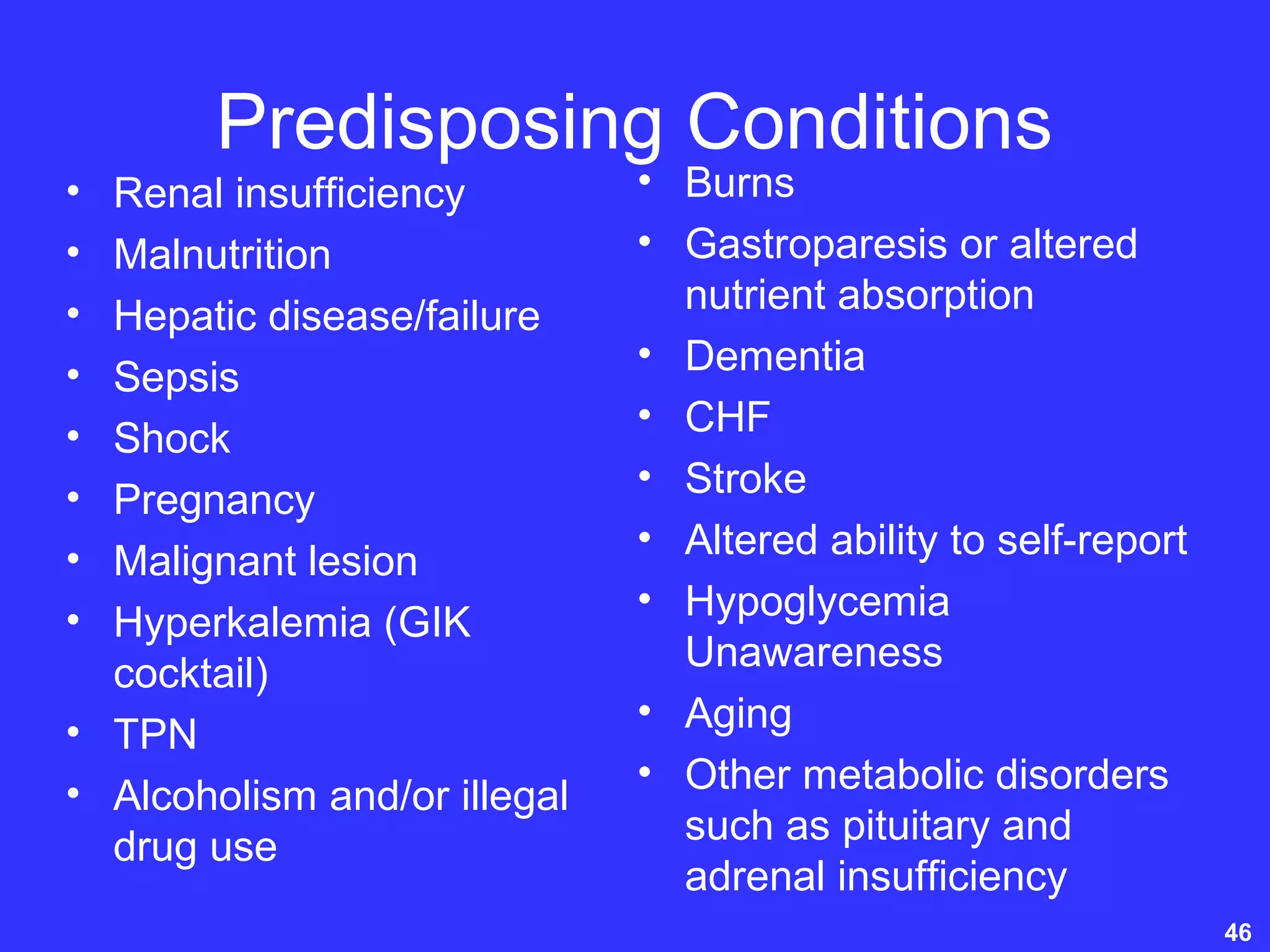
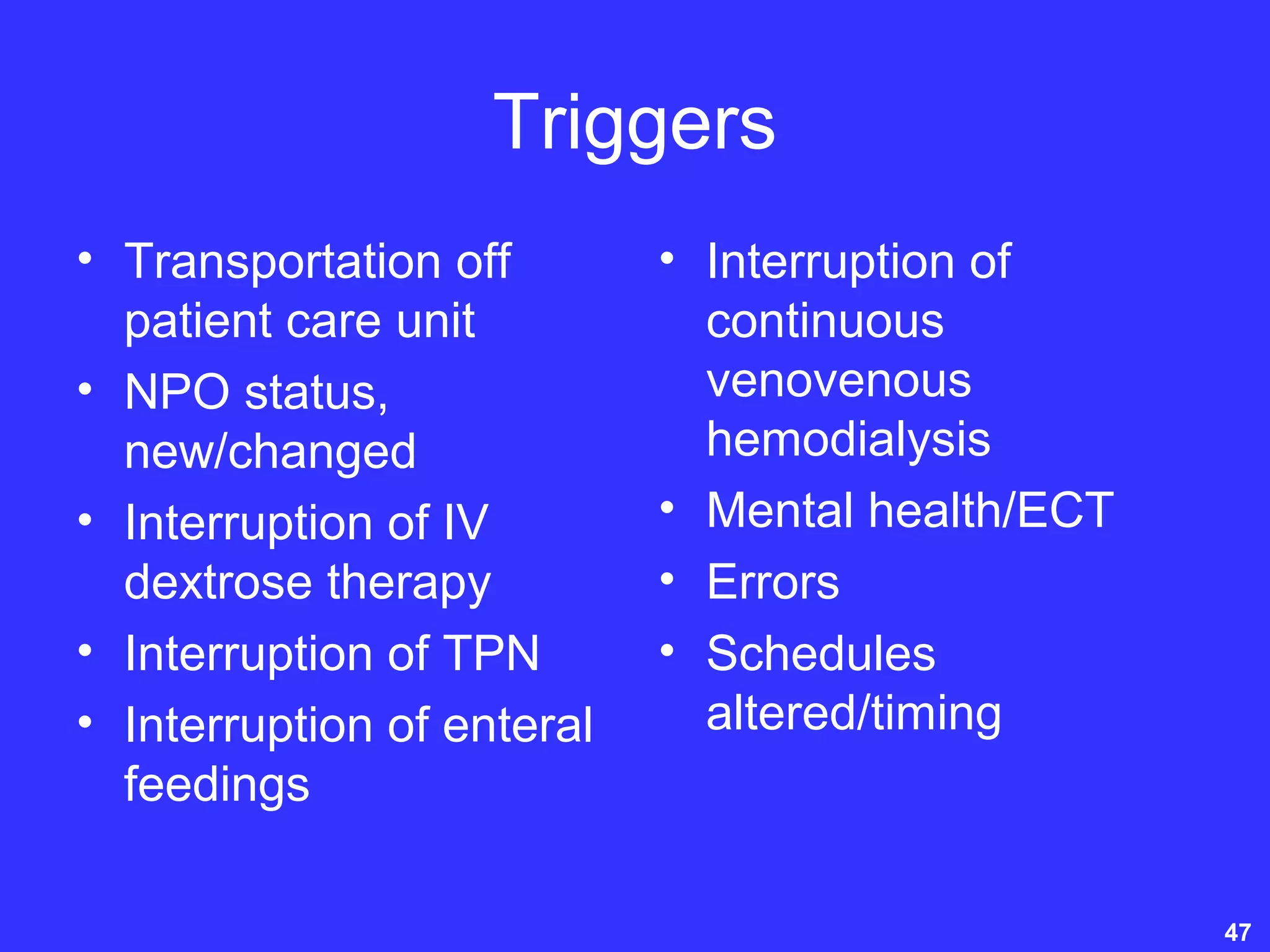
This document discusses the pathophysiology, treatment, and management of hyperglycemic crises including diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic nonketotic syndrome (HHNS) in acute care settings. It covers topics such as the treatment modalities for optimal glycemic management including insulin administration, fluid and electrolyte replacement, nutrition management, and hypoglycemia prevention. The document provides details on the causes, signs and symptoms, and treatment approaches for DKA and HHNS including insulin therapy, fluid resuscitation, electrolyte replacement, and management of any underlying conditions or complications.