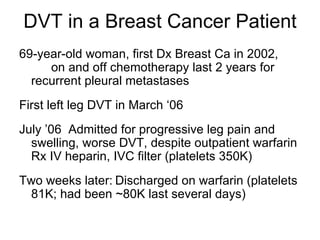
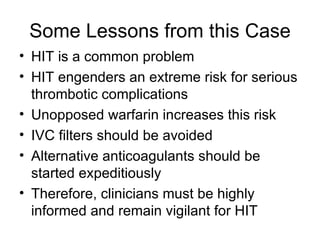
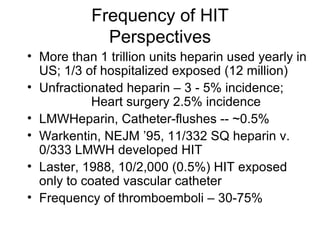
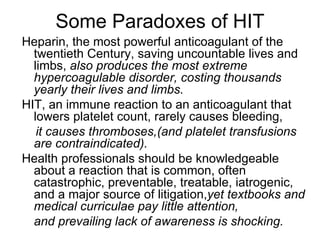
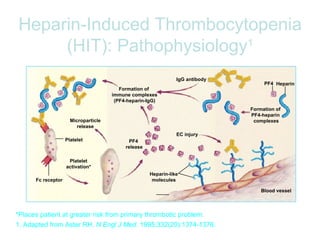
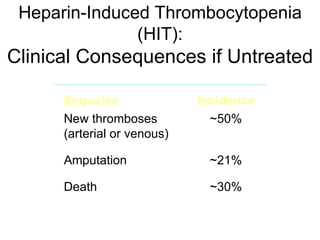
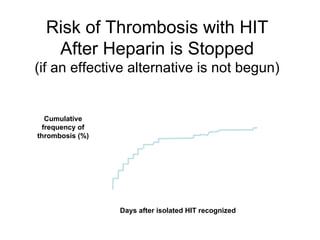
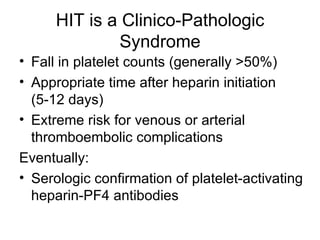
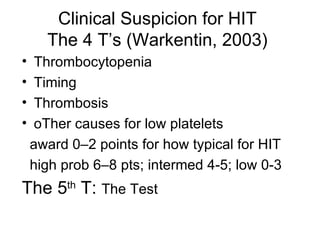
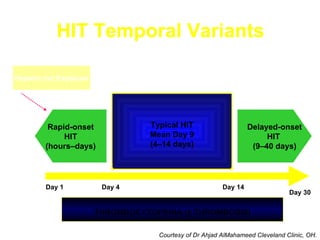
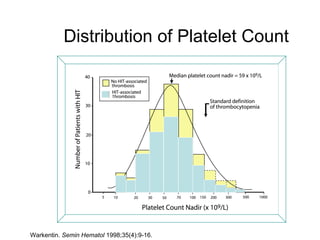
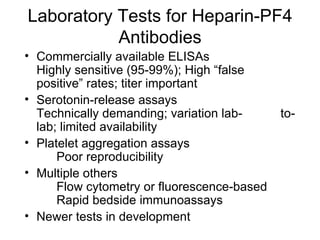
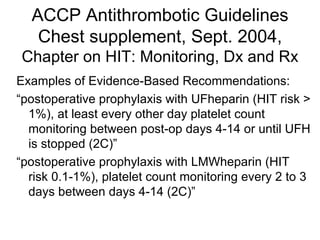
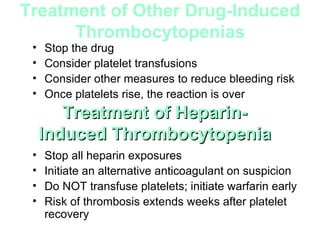
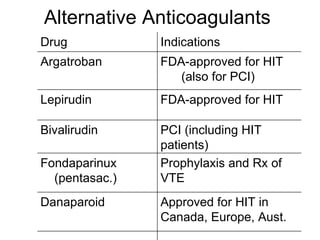
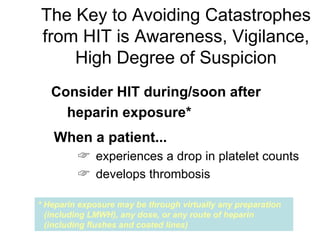
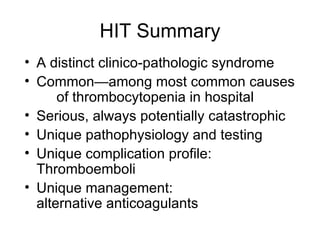
Heparin-induced thrombocytopenia (HIT) is a common and potentially catastrophic complication of heparin therapy that can lead to thromboembolic events like DVT or death. It is important for clinicians to be aware of HIT, as it requires unique management compared to other causes of thrombocytopenia, including stopping heparin and starting alternative anticoagulants without delay. Laboratory tests can help confirm the diagnosis but clinical suspicion is also important given the serious risks of untreated HIT.