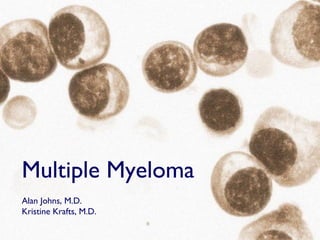
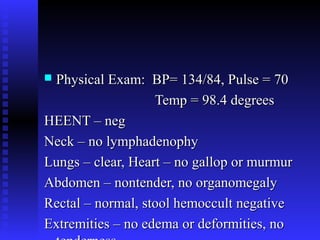
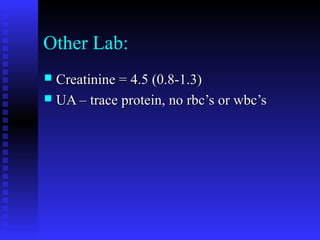
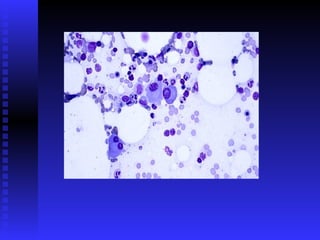
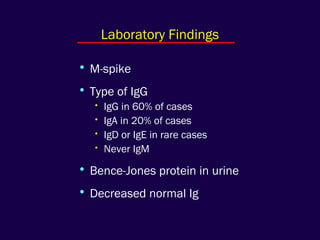
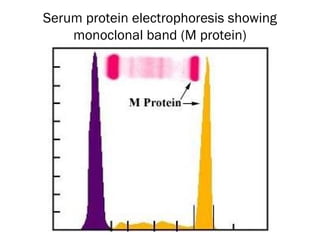
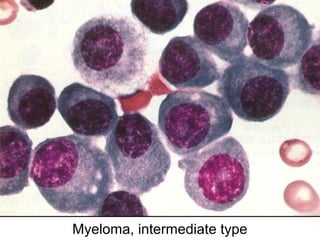
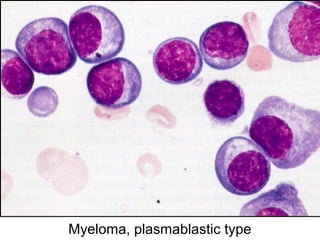
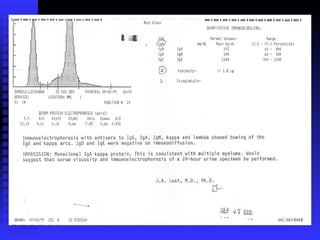
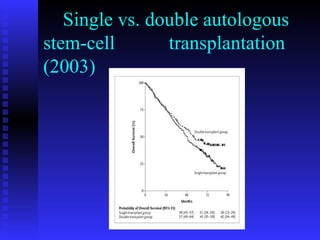
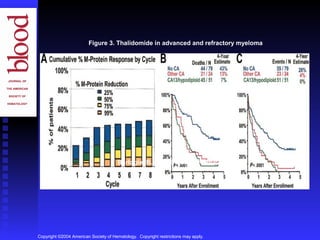
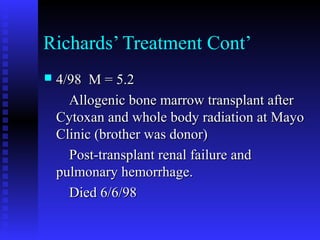
Richard, a 51-year-old male, presented with epigastric distress, weight loss, anemia, and renal failure. Bone marrow testing revealed he had multiple myeloma, a cancer of plasma cells which produces monoclonal proteins that can cause organ and tissue damage. He was diagnosed based on his bone marrow containing over 20% plasma cells and laboratory findings showing monoclonal proteins. Multiple myeloma is typically treated with chemotherapy like melphalan and prednisone or stem cell transplants, though newer agents like thalidomide and bortezomib have improved outcomes in some patients.