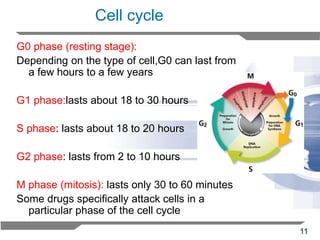
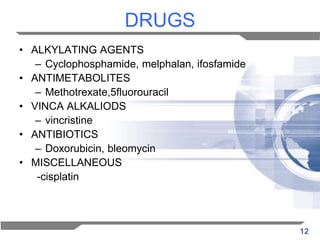
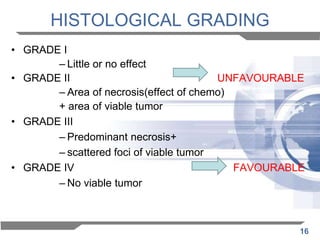
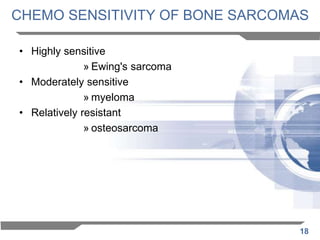
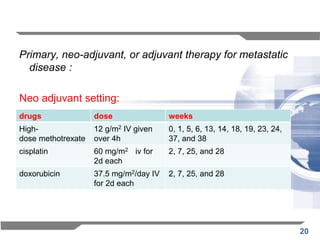
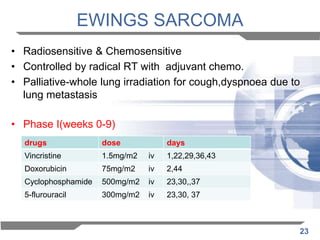
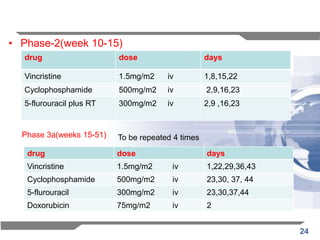
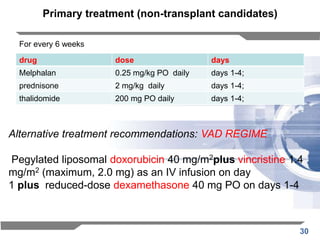
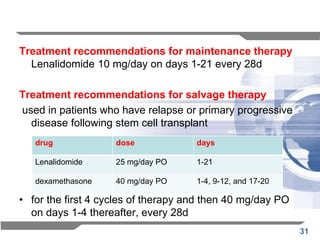
This document discusses the use of chemotherapy in orthopaedics, specifically for musculoskeletal tumors. It provides information on the different types and goals of chemotherapy, including neoadjuvant, adjuvant, and palliative chemotherapy. It discusses the mechanism of action, types of drugs used, and side effects. Treatment recommendations are provided for specific cancers like osteosarcoma, Ewing's sarcoma, multiple myeloma, and metastatic bone tumors. The overall goal of chemotherapy for these cancers is curative treatment, disease control, or palliation to improve quality of life.