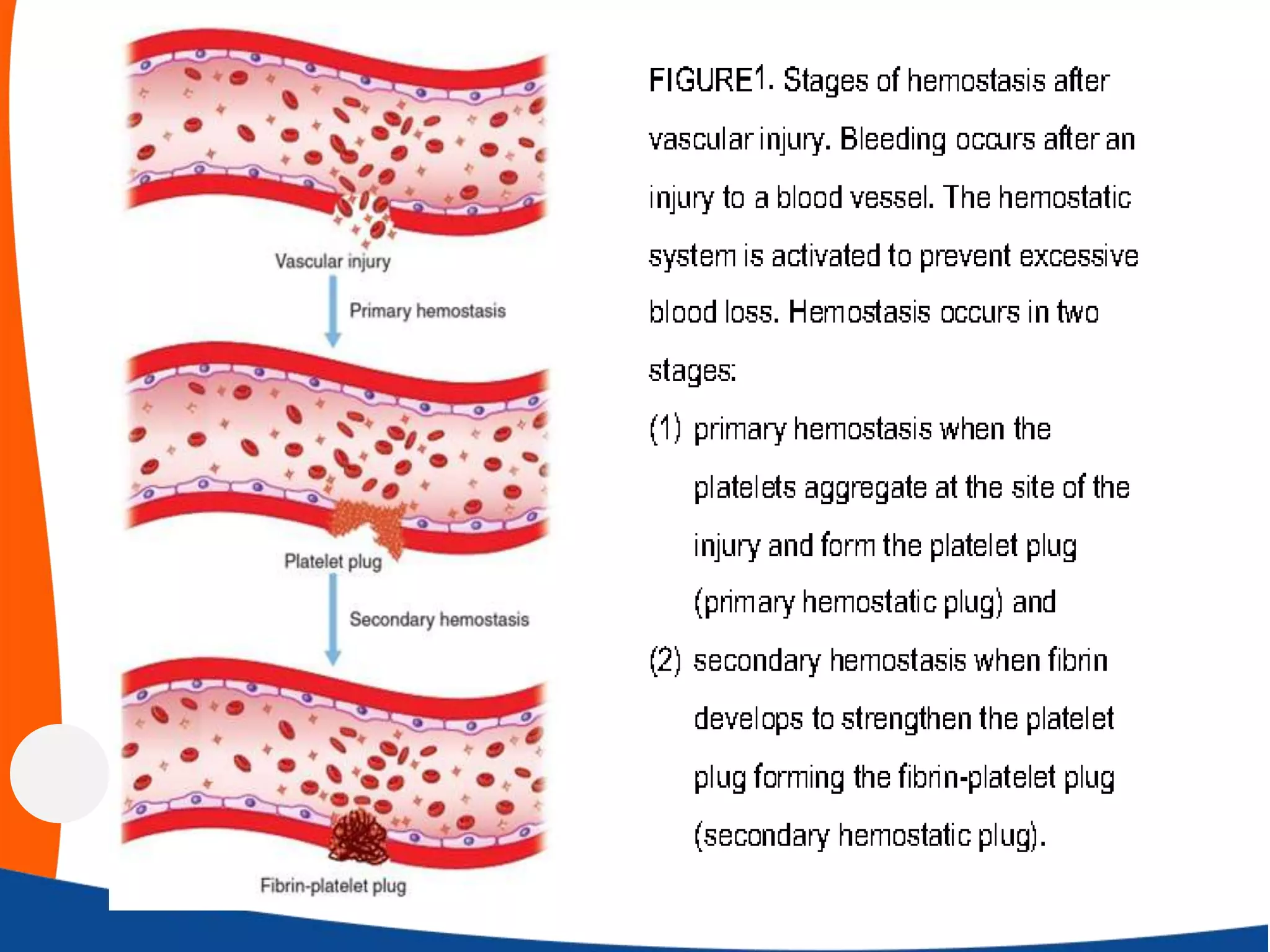
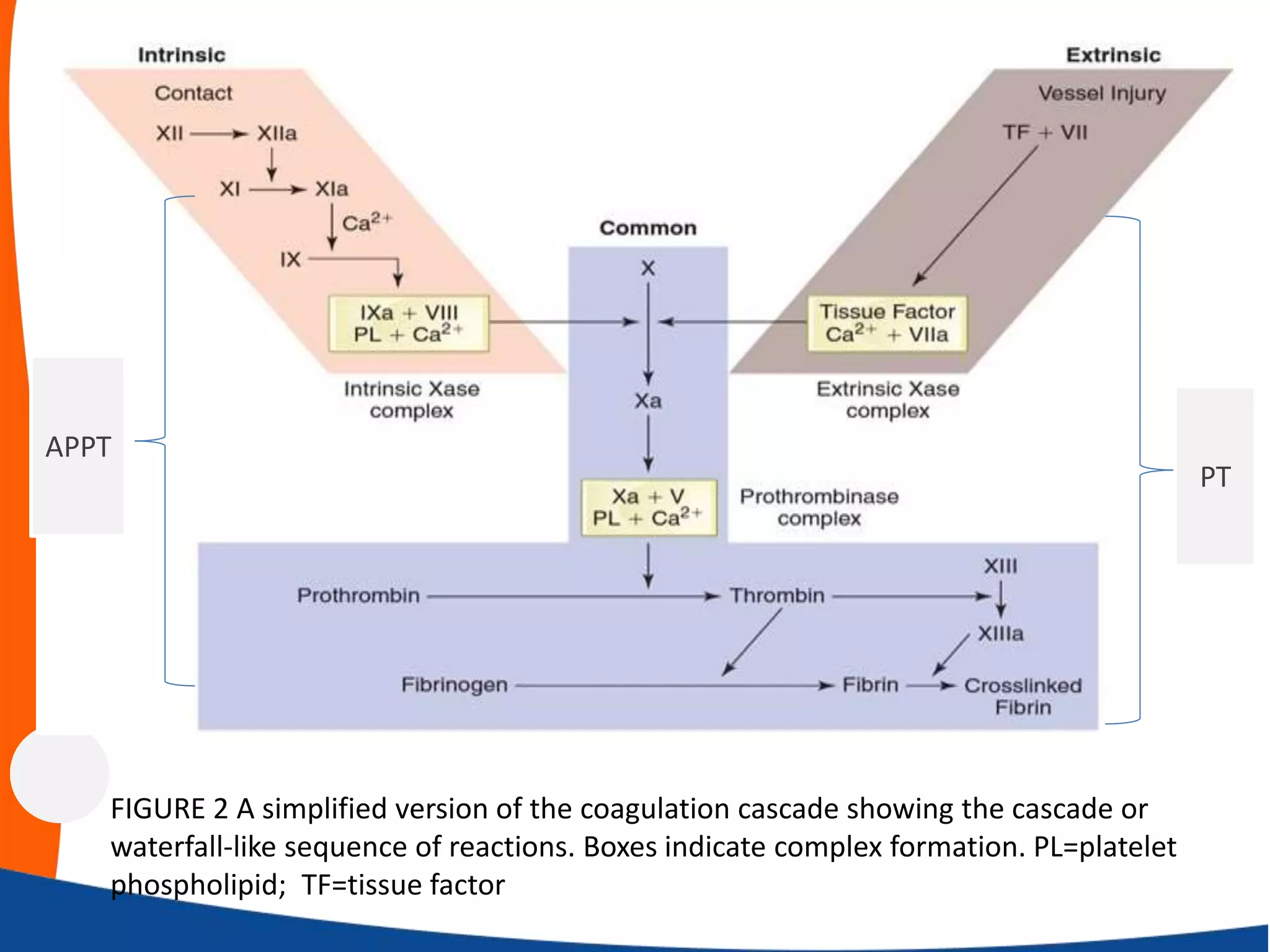
This document provides an overview of haemostasis (the process of stopping bleeding from damaged blood vessels). It discusses the key components involved - the vessel wall, platelets, and coagulation factors - and how they interact. The vessel wall normally prevents clotting but releases substances upon injury that activate platelets and the coagulation cascade. Platelets form a primary plug which is stabilized by fibrin formed from coagulation factors. Tests are used to identify defects in haemostasis involving vessels, platelets or coagulation.